- - In the present OE Original, we systematically examined evidence from randomized controlled trials (RCTs) regarding the clinical and safety outcomes of patients undergoing robotic arm-assisted unicompartmental knee arthroplasty (UKA) compared to those undergoing conventional UKA.
- - Five studies were included. These studies followed 3 patient cohorts and investigated 3 robotic systems: Mako, Navio, and Acrobot robotic systems.
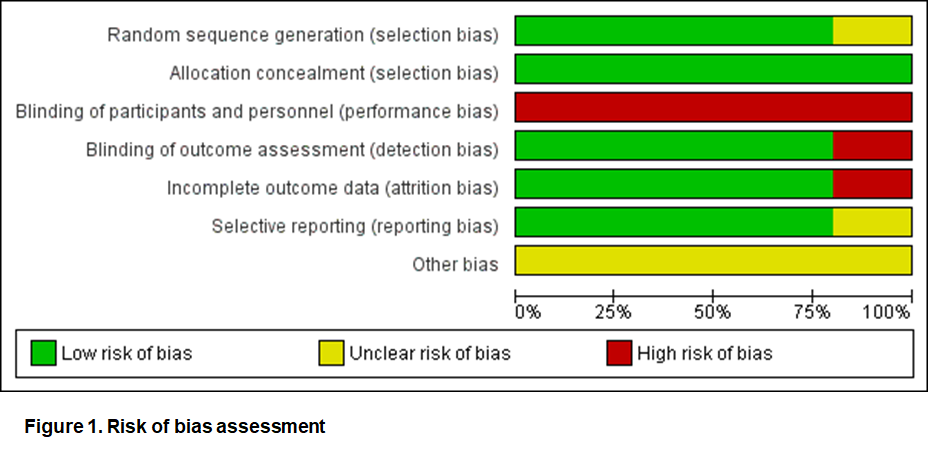
- - Results from the included RCTs might be subject to performance bias as it was not possible to blind participants due to differences in procedures between robotic-assisted UKA and conventional UKA. Sponsorship bias might also exist due to the fact that all of the included RCTs were sponsored by the manufacturers of the robotic systems.
- - Our narrative summary showed that robotic-assisted UKA is neither superior nor inferior to conventional UKA in terms of function and pain outcomes [i.e., OKS (Oxford knee score), FJS (Forgotten joint score), WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain, VAS (visual analogue scale) pain] as well as safety outcomes (i.e., revision).
- - More RCTs, with high methodological quality, large sample size, and preferably funded by a third party other than the manufacturers of the robotic systems, are needed.
Unicompartmental knee arthroplasty (UKA), an alternative to total knee arthroplasty (TKA), is considered as a minimally invasive approach which selectively replaces the damaged knee compartment caused by end-stage, symptomatic osteoarthritis (OA) in order to maximally preserve normal anatomy (Confalonieri et al., 2005; Mittal et al., 2020). Evidence from the body of literature suggests better results for UKA over TKA in a number of outcomes, such as length of hospital stay and functional patient reported outcome measure (PROM) scores (Wilson et al., 2019).
Several methods of surgical assistance such as robotic support systems have been developed with the aim of increasing the accuracy in positioning of the implants, improving clinical results, and reducing complications among patients undergoing UKA. Chen et al. (2018) classified the robotic support systems used in orthopedic surgery based on direct and indirect action and according to the mechanism of cutting, including autonomous, haptic, and boundary control.
For instance, the MAKO robotic system for UKA developed by Stryker is classified as direct and haptic, meaning the robot cuts the bone under the guidance of a human hand within a haptic boundary (Chen et al., 2018). The NAVIO robotic system for UKA developed by Smith & Nephew is, on the other hand, categorized as direct and boundary control -- the latter indicates that the system will be shut off when boundaries are exceeded (Chen et al., 2018). The Acrobot system is considered a semi-active system which was designed to restrict what can be done surgically through feedback rather than an autonomous system like the MAKO and NAVIO systems (Chen et al., 2018). The Acrobot system is no longer on the market as Stryker purchased all of its patents and technology (Chen et al., 2018).
A number of evidence summary and syntheses comparing UKA using robotic arm-assisted UKA with conventional UKA have been published recently (e.g., Gaudiani et al., 2020; Iturriaga et al., 2020; Negrin et al., 2021; Sun et al., 2021; F. Zhang et al., 2019; P. Zhang et al., 2021). In the present OE Original, we conduct a systematic review to examine evidence from randomized controlled trials (RCTs) with regard to the clinical and safety outcomes of patients undergoing robotic arm-assisted UKA vs. those undergoing conventional UKA.
Methods
Ovid MEDLINE, Ovid EMBASE, Cochrane Controlled Register of Trials (CENTRAL), and OrthoEvidence were searched from inception to December 1, 2021 with both indexed terms and free text terms with regard to robotic surgical procedures and UKA. Reference lists and existing systematic reviews (i.e., Gaudiani et al., 2020; Iturriaga et al., 2020; Negrin et al., 2021; Sun et al., 2021; Zhang et al., 2019; Zhang et al., 2021) were searched to identify additional eligible studies.
Eligible studies were RCTs comparing the robotic arm-assisted UKA with conventional UKA published in English. Studies conducted in cadavers were excluded. Conference abstracts were also excluded.
We adopted the Cochrane risk-of-bias tool to determine the risk of bias of the included RCTs, respectively. Two reviewers independently worked on the systematic review processes, such as study screening, selection, data extraction, and risk of bias assessment. Any disagreement was resolved by consulting a third reviewer.
Results
1. Characteristics of included RCTs
In total, 552 records were retrieved and screened. Five studies were determined eligible (Banger et al., 2021; Batailler et al., 2021; Bell et al., 2016; Cobb et al., 2006; Gilmour et al., 2018). The characteristics of these 5 studies were presented in Table 1.
Three RCTs conducted in the United Kingdom (UK) (Banger et al., 2021; Bell et al., 2016; Gilmour et al., 2018) followed the same patient cohort at different periods in time. These 3 RCTs investigated the robotic support systems developed by MAKO Surgical Corporation (now Stryker) and were also funded by Stryker.
Cobb et al. (2006), which was funded by Acrobot Co Ltd, investigated the Acrobot system, which was no longer on the market due to the acquisition by MAKO Surgical Corporation (now Stryker).
The RCT conducted by Batailler et al. (2021) in France was funded by Smith & Nephew and focused on the BlueBelt Navio image-free robotic surgical system.
The RCT series on the MAKO robotic-arm interactive orthopedic system (Banger et al., 2021; Bell et al., 2016; Gilmour et al., 2018) explicitly stated the surgical technique used in the control group, which was Oxford phase 3 UKA using standard manual phase 3 instrumentation with implantation of the RESTORIS MCK fixed-bearing unicompartmental knee replacement.
The implants (Journey II Uni) used by Batailler et al. (2021) were cemented implants with a distal cut technique for the femur and a fixed bearing polyethylene. Cobb et al. (2006) mentioned the Oxford UKA vaguely.
Table 1. Characteristics of included RCTs | |||||||
Study ID | Country | Funding Source | No. of Patients at Randomization | No. of Patients Analyzed | Age (years) | Intervention | Control |
Bell 2016 | UK | MAKO Surgical Corporation (now Stryker) | 139 | 120 | Intervention: mean: 62.5 (SD: 6.9); Control: 61.7 (7.9) | Robotic arm-assisted UKA using the MAKO robotic-arm interactive orthopedic system | Oxford phase 3 UKA |
Gilmour 2018 | UK | MAKO Surgical Corporation (now Stryker) | 139 | 112 | Intervention: 61.8 (7.84); Control: 62.6 (7.13) | Robotic arm-assisted UKA using the MAKO robotic-arm interactive orthopedic system | Oxford phase 3 UKA |
Banger 2021 | UK | MAKO Surgical Corporation (now Stryker) | 139 | 104 | Not Reported | Robotic arm-assisted UKA using the MAKO robotic-arm interactive orthopedic system | Oxford phase 3 UKA |
Batailler 2021 | France | Smith & Nephew | 66 | 66 | Intervention: 65.6 (7.9); Control: 67.1 (8.1) | Robotic arm-assisted UKA using the BlueBelt Navio image-free robotic surgical system | Conventional UKA |
Cobb 2006 | UK | Acrobot Co Ltd | 28 | 28 | Intervention: 69.8 (range: 58 to 78); Control: 70.4 (62 to 79) | Robotic arm-assisted UKA using the Acrobot system | Conventional UKA |
UK: United Kingdom; SD: standard deviation; UKA: unicompartmental knee arthroplasty | |||||||
The risk of bias assessment was shown in Figure 1. Blinding participants seemed not to be possible as the procedures (e.g., preoperative CT scans, additional incisions required for the trackers in the robotic-assisted technique.) were different between robotic arm-assisted surgery and conventional surgery.
We considered surgeons’ experience in the “Other bias” item. None of the included RCTs explicitly stated the extent to which the surgeons were familiar with the robotic surgical systems under investigation. However, all the RCTs indicated that the surgeons had considerable experience in the conventional UKA.
2. Evidence Synthesis
Only narrative summary was carried out due to the following reasons: I) Out of the 5 included RCTs, there were only 3 patient cohorts involving 3 different robotic surgery support systems. The Acrobat system was no longer on the market. II) The differences in follow-up duration could not be ignored as clinical outcomes were followed up at 6 or 18 weeks (Cobb et al., 2006), 6 months (Batailler et al., 2021), 2 years or 5 years (Banger et al., 2021; Gilmour et al., 2018) for the 3 patient cohorts, respectively. The narrative summary of results from included RCTs were presented in Table 2.
Table 2. Result summary from included RCTs* | ||||
| Cobb 2006 (Acrobot) | Batailler 2021 (Navio) | Gilmour 2018 (Mako) | Banger 2021 (Mako) |
KSS | 1. Total At 6 or 18 weeks**, Robotic (N = 13): 65.2 (18.36); Conventional (N = 14): 32.5 (27.46); P = 0.004 (change from baseline) | 1. Knee score At 6 months, Robotic (N = 33): 91.9 (10.2); Conventional (N = 33): 88.8 (8.9); P = 0.22 2. Function score At 6 months, Robotic (N = 33): 87.2 (13.7); Conventional (N = 33): 81.3 (12); P = 0.074 | 1. Total At 2 years, Robotic (N = 58): 105.5 (27.4); Conventional (N = 54): 102.8 (24.6); P = 0.581 | 1. Knee score (mean IQR) At 5 years, Robotic (N = 55): 89 (80 to 97); Conventional (N = 49): 88 (83.75 to 98); P = 0.817 2. Function score At 5 years, Robotic (N = 55): 80 (60 to 90); Conventional (N = 49): 90 (70 to 90); P = 0.636 3. Total At 5 years, Robotic (N = 55): 167 (139.75 to 185); Conventional (N = 49): 177 (145 to 188.25); P = 0.532 |
OKS | Not Reported | Not Reported | At 2 years, Robotic (N = 58): 19.5 (11.3); Conventional (N = 54): 21 (8.5); P = 0.986 (median IQR) | At 5 years, Robotic (N = 55): 40 (35 to 44); Conventional (N = 49): 41 (34.75 to 44); P = 0.812 (median IQR) |
FJS | Not Reported | At 6 months, Robotic (N = 33): 76.8 (20.4); Conventional (N = 33): 68.1 (21.1); P = 0.1 | At 2 years, Robotic (N = 58): 55.2 (58.5); Conventional (N = 54): 54.1 (42.2); P = 0.937 (mean IQR) | At 5 years, Robotic (N = 55): 50 (22.9 to 85.4); Conventional (N = 49): 52 (28.1 to 72.9); P = 0.784 (median IQR) |
Pain | 1. WOMAC pain At 6 or 18 weeks**, Robotic (N = 13): 8 (3); Conventional (N = 14): 6 (2); no significance (change from baseline) | Not Reported | 1. VAS pain At 2 years, Robotic (N = 58): 52.7 (24.6); Conventional (N = 54): 55.1 (18.7); P = 0.575 | 1. VAS pain At 5 years, Robotic (N = 55): 18.6 (22.6); Conventional (N = 49): 15.9 (22.8); P = 0.454 |
Revision | Not Reported | At 6 months, Robotic (N = 33): 1 (3%); Conventional (N = 33): 0; P = 0.99 (No. of events, %) | At 2 years, Robotic (N = 58): 0; Conventional (N = 54): 2 (3.7%); P not reported (No. of events, %) | At 5 years, Robotic (N = 55): 0; Conventional (N = 49): 2 (4%); P = 0.476 (No. of events, %) |
* Unless specified, data were represented as mean and standard deviation; ** The study did not specify the exact follow-up time point; KSS: Knee society score; N: Number of patients; IQR: Interquartile range; OKS: Oxford knee score; FJS: Forgotten joint score; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; VAS: Visual analogue scale | ||||
2.1 Knee society score
Knee society score (KSS) is a clinical evaluation system, consisting of 2 components -- knee score and function score (Insall et al., 1989). The knee score, including pain, stability, and range of motion, evaluates the knee clinically via the physical examination, while the function score including walking distance and the act of climbing and descending stairs assesses the examinee's functionality (Martimbianco et al., 2012). KSS has been one of the most popular methods of reporting outcomes in patients undergoing total and partial knee arthroplasty.
Four studies reported KSS scores (Banger et al., 2021; Batailler et al., 2021; Cobb et al., 2006; Gilmour et al., 2018). Only Cobb et al. (2006) identified a statistically significant difference in the total KSS scores between Acrobot -assisted UKA and conventional UKA at 6 or 18 weeks after surgery, whereas none of the remaining RCTs found any statistically significant difference in the KSS knee scores, function scores, or total KSS scores between robotic arm-assisted UKA (i.e., the Mako or Navio system) and conventional UKA at 6 months, 2 years, or 5 years after surgery (Table 2).
2.2 Oxford knee score
Oxford knee score (OKS) was developed to evaluate the outcomes of knee arthroplasties reported by patients so as to minimize potential bias introduced by operating surgeons when evaluating the results themselves (Dawson et al., 1998).
Two studies reported OKS scores (Banger et al., 2021; Gilmour et al., 2018). No significant differences were identified between the Mako robotic arm-assisted UKA and conventional UKA at 2 years or 5 years after surgery (Table 2).
2.3 Forgotten joint score
Forgotten joint score (FJS) features the concept that “the ability to forget the artificial joint in everyday life can be regarded as the ultimate goal in joint arthroplasty resulting in the greatest possible patient satisfaction” (Behrend et al., 2012).
Three studies reported FJS scores (Banger et al., 2021; Batailler et al., 2021; Gilmour et al., 2018). None of them found any significant difference between robotic arm-assisted UKA (i.e., the Mako or Navio system) and conventional UKA at 6 months, 2 years, or 5 years after surgery (Table 2).
2.4 Pain
Banger et al. (2021) and Gilmour et al. (2018) reported pain on the visual analog scale (VAS), while Cobb et al. (2006) reported the Western Ontario and McMaster Universities index (WOMAC) pain score. No significant differences were found between the Robotic UKA and conventional UKA for either of the RCTs (Table 2).
2.5 Revision
Three studies reported FJS scores (Banger et al., 2021; Batailler et al., 2021; Gilmour et al., 2018). There were no significant differences in the incidence of revision between robotic arm-assisted UKA (i.e., the Mako or Navio system) and conventional UKA at 6 months, 2 years, or 5 years after surgery (Table 2).
2.6 Other outcomes
Banger et al. (2021) also reported outcomes relating to quality of life (QoL) using the EuroQol-five-dimension (EQ-5D) VAS and EuroQol-five dimension three-level (EQ-5D-3L). No significant differences were identified between Mako robotic-assisted UKA and conventional UKA at 5 years post surgery (EQ-5D VAS: P = 0.316; EQ-5D-3L: P = 0.353).
Bell et al. (2016) focused on the accuracy of component positioning instead of clinical outcomes and found that robotic-assisted UKA using the Mako system resulted in an improved accuracy of implant positioning as opposed to that of conventional UKA.
Discussion
In the present OE Original, we systematically reviewed RCT evidence regarding the use of robotic-assisted UKA compared to conventional UKA.
Our systematic literature search suggests that RCT evidence is limited as only 5 studies following up with 3 patient cohorts and investigating 3 robotic systems were identified. The 3 systems are Mako, Navio, and Acrobot systems. The latter one was off the market.
Results from these included RCTs might be subject to performance bias as it was not possible to blind participants due to differences in procedures between robotic-assisted UKA and conventional UKA. Sponsorship bias might also exist due to the fact that all of the included RCTs were sponsored by the manufacturers of the robotic systems.
Result summary of the included RCTs showed that robotic-assisted UKA is neither superior nor inferior to conventional UKA in terms of function and pain outcomes [i.e., OKS (Oxford knee score), FJS (Forgotten joint score), WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) pain, VAS (visual analogue scale) pain] as well as safety outcomes (i.e., revision).
In the past year, a number of systematic reviews and meta-analyses comparing UKA using robotic arm-assisted UKA with conventional UKA have been published (Negrin et al., 2021; Sun et al., 2021; Zhang et al., 2021). The 3 systematic reviews searched databases similar to ours till June 2020. All of them included both RCTs and non-randomized studies on intervention effects (NRSIs). By including NRSIs, these systematic reviews are likely to be more informative compared to this OE Original including only RCTs. However, NRSIs usually suffer higher risk of bias than RCTs. Therefore, systematic reviews of RCTs are more likely to provide unbiased information about the effects of health interventions than those including NRSIs (Higgins et al. 2021). Results should always be cautiously interpreted when NRSIs are included in systematic reviews and meta-analyses.
Conclusions on function and pain outcomes from our narrative summary of RCTs only are similar to the results of quantitative synthesis conducted by Zhang et al. (2021), which found no significant differences between robotic-assisted UKA and conventional UKA in outcomes such as KSS and pain. Based on their narrative synthesis, Negrin et al. (2021) also concluded that although accuracy was improved by the robotic system, yet current evidence did not support significant improvements in clinical outcomes after robotic-assisted UKA.
Sun et al. (2021), summarizing 10 studies (RCTs and NRSIs), found that robotic-assisted UKA had significantly lower risk of revision [relative risk (RR): 0.42, 95% confidence interval (CI): 0.20 to 0.86] than conventional UKA, whereas Zhang et al. (2021), summarizing 4 studies (all of them were synthesized by Sun et al.), showed no significant differences (RR: 0.88; 95% CI: 0.43 to 1.82). In the present OE Original, we identified no statistical significance. Despite the discrepancy, robotic-assisted UKA could be considered safe in terms of risk of revision.
Conclusion
Current RCT evidence suggests that robotic-assisted UKA is a safe procedure but neither superior or inferior to conventional UKA in function and pain outcomes. More RCTs, with high methodological quality, large sample size, and preferably funded by a third party other than the manufacturers of the robotic systems, are warranted.
References
Banger, M., et al. (2021). Robotic arm-assisted versus conventional medial unicompartmental knee arthroplasty: five-year clinical outcomes of a randomized controlled trial. The bone & joint journal, 103-B(6), 1088-1095. doi:http://dx.doi.org/10.1302/0301-620X.103B6.BJJ-2020-1355.R2
Batailler, C., et al. (2021). No difference of gait parameters in patients with image-free robotic-assisted medial unicompartmental knee arthroplasty compared to a conventional technique: early results of a randomized controlled trial. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. doi:http://dx.doi.org/10.1007/s00167-021-06560-5
Behrend, H., et al. (2012). The “Forgotten Joint” as the Ultimate Goal in Joint Arthroplasty: Validation of a New Patient-Reported Outcome Measure. The Journal of Arthroplasty, 27(3), 430-436.e431. doi:https://doi.org/10.1016/j.arth.2011.06.035
Bell, S. W., et al. (2016). Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty. Journal of Bone and Joint Surgery - American Volume, 98(8), 627-635. doi:http://dx.doi.org/10.2106/JBJS.15.00664
Chen, A. F. et al. (2018). Robotic Technology in Orthopaedic Surgery. The Journal of Bone and Joint Surgery, 100 (22), 1984-1992. doi: 10.2106/JBJS.17.01397.
Cobb, J., et al. (2006). Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br, 88(2), 188-197. doi:10.1302/0301-620x.88b2.17220
Confalonieri, N., et al. (2005). Mini-invasive computer assisted bi-unicompartimental knee replacement. Int J Med Robot, 1(4), 45-50. doi:10.1002/rcs.56
Dawson, J., et al. (1998). Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br, 80(1), 63-69. doi:10.1302/0301-620x.80b1.7859
Gaudiani, M. A., et al. (2020). Robotic-Assisted versus Manual Unicompartmental Knee Arthroplasty: Contemporary Systematic Review and Meta-analysis of Early Functional Outcomes. The journal of knee surgery. doi:http://dx.doi.org/10.1055/s-0040-1701455
Gilmour, A., et al. (2018). Robotic-Arm–Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. Journal of arthroplasty, 33(7), S109-S115. doi:10.1016/j.arth.2018.02.050
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook
Insall, J. N., et al. (1989). Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res(248), 13-14.
Iturriaga, C., et al. (2020). Robotic-Assisted Versus Manual Unicompartmental Knee Arthroplasty: A Systematic Review. Surgical technology international, 37, 275-279.
Martimbianco, A. L., et al. (2012). Reliability of the "American Knee Society Score" (AKSS). Acta Ortop Bras, 20(1), 34-38. doi:10.1590/s1413-78522012000100007
Mittal, A., et al. (2020). Unicompartmental knee arthroplasty, an enigma, and the ten enigmas of medial UKA. J Orthop Traumatol, 21(1), 15. doi:10.1186/s10195-020-00551-x
Motesharei, A., et al. (2018). A comparison of gait one year post operation in an RCT of robotic UKA versus traditional Oxford UKA. Gait and Posture, 62, 41-45. doi:http://dx.doi.org/10.1016/j.gaitpost.2018.02.029
Murray, D. W., et al. (2015). Unicompartmental knee arthroplasty: is the glass half full or half empty? The bone & joint journal, 97-B(10 Suppl A), 3-8. doi:10.1302/0301-620X.97B10.36542
Negrin, R., et al. (2021). Robotic-assisted surgery in medial unicompartmental knee arthroplasty: does it improve the precision of the surgery and its clinical outcomes? Systematic review. Journal of Robotic Surgery, 15(2), 165-177. doi:http://dx.doi.org/10.1007/s11701-020-01162-8
Sun, Y., et al. (2021). Does robotic-assisted unicompartmental knee arthroplasty have lower complication and revision rates than the conventional procedure? A systematic review and meta-analysis. BMJ Open, 11(8), e044778. doi:http://dx.doi.org/10.1136/bmjopen-2020-044778
Wilson, H. A., et al. (2019). Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ, 364, l352. doi:10.1136/bmj.l352
Zhang, F., et al. (2019). Robotic arm-assisted vs conventional unicompartmental knee arthroplasty: A meta-analysis of the effects on clinical outcomes. Medicine, 98(35), e16968. doi:http://dx.doi.org/10.1097/MD.0000000000016968
Zhang, P., et al. (2021). Comparison of robotic-assisted versus conventional unicompartmental knee arthroplasty for the treatment of single compartment knee osteoarthritis: A meta-analysis. International Journal of Medical Robotics and Computer Assisted Surgery, 17(1), 1-11. doi:http://dx.doi.org/10.1002/rcs.2170
ere.




 LOGIN
LOGIN

Join the Conversation
Please Login or Join to leave comments.