Improving Outcomes for Open Fractures: An Orthoplastic Approach to Care

Improving Outcomes for Open Fractures: An Orthoplastic Approach to Care
Vol: | Issue: | Number: | ISSN#: 2563-5972
October 1, 2021 | Article No. 71

Improving Outcomes for Open Fractures: An Orthoplastic Approach to Care
October 1, 2021 | Article No. 103
Ayesha Siddiqua MSc, PhD
Mohit Bhandari MD, PhD

Dr. Bradley Petrisor is an orthopaedic surgeon and a professor in the Department of Surgery at McMaster University. His research interests include functional outcome scoring in foot and ankle trauma, trauma outcomes and fluid irrigation techniques in the management of open fractures.
Insights
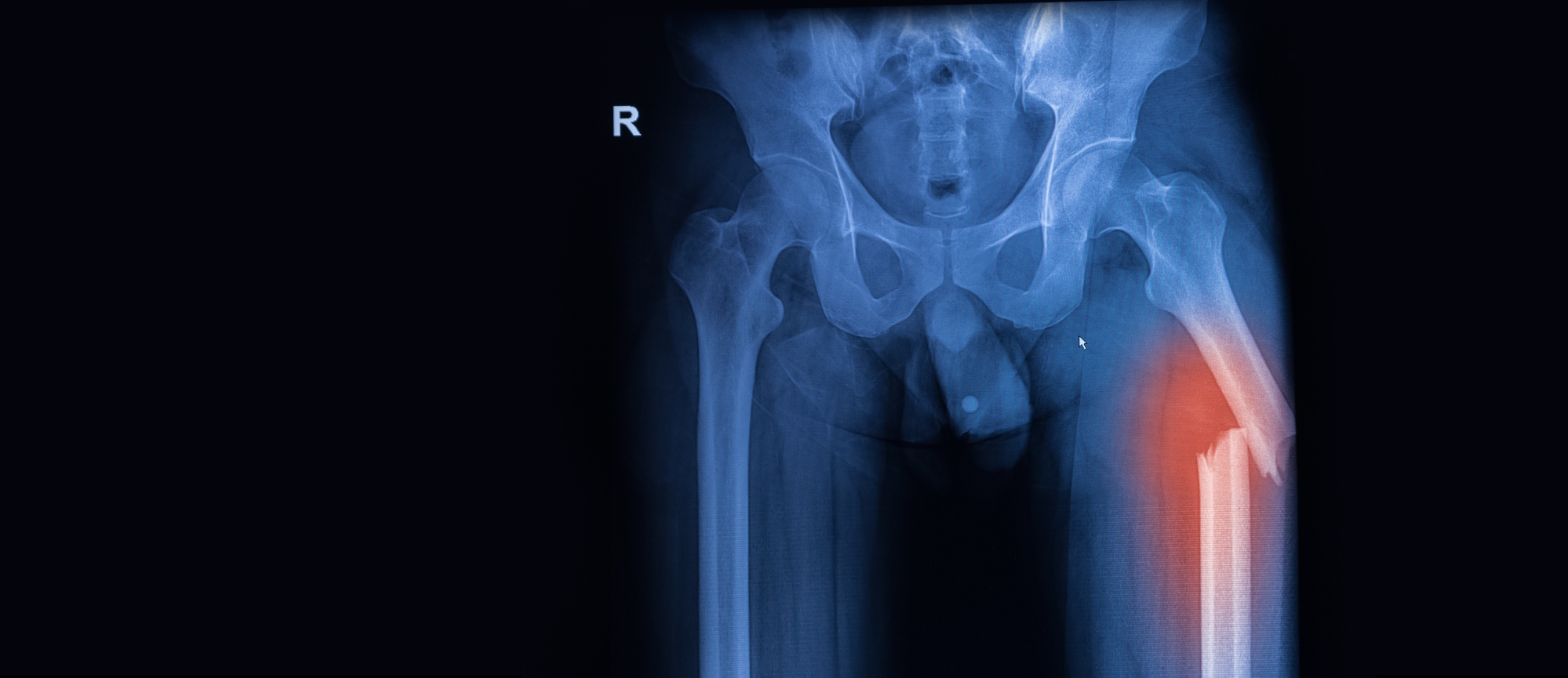
- Open fractures are common orthopaedic injuries around the world
- These fractures are at significant risk of infection due in part to broken skin but also to the occurrence of potentially significant soft tissue damage and periosteal stripping - early management to prevent this complication is recommended
- Given the nature of open fractures that are characterized by soft tissue damage, an orthoplastic approach has been increasingly adopted across many settings
- While there is considerable evidence to support an orthoplastic approach in terms of improved patient outcomes, there is still lack of consensus regarding several technical aspects of this approach
- The timing of soft tissue coverage, whether to conduct this within a single or staged procedure, remains a key controversy
- Several informational and guidance documents are available to inform the implementation of an orthoplastic approach, which need to be customized to the local context of practice

“A 15-year review of epidemiologic factors of open fractures in adults, reports the incidence was 30.7 per 100,000 persons per year. Motor vehicle accidents are the most common cause of open, lower extremity fractures and are responsible for 34.1% of these injuries. The overall average age of occurrence is 45.5 years, but in general, the incidence declines in males and increases in females with age…Open phalanx fractures are the most common open fractures accounting for more than 45% of all open injuries.”
Sop & Sop
(2021) (1)

“Open tibia fractures, in particular, have received increased attention due to their prevalence and severity. These fractures are the second-most common open bone injury, occurring in nearly 1-quarter of all tibial diaphyseal fractures, with estimates of 17 to 23 open tibia fractures per 100,000 person years. Additionally, approximately 60% of open tibial fractures result from higher energy injuries, which are associated with severe soft tissue lesions.”
Miclau
(2020) (2)

“It has been 20 years since Gopal and Smith et al. published their remarkable achievements in dealing with severe open fractures of the tibia by radical orthoplastic approach. However, similar studies have rarely been reported in recent years. This is mainly because severe open fractures (referred to as Gustilo IIIb or IIIc injuries), which often lead to large soft tissue defects and high risk of infection, are still a challenge for reconstructive surgeons. Although various methods and standards have been used for managing open fractures in the lower limb, the salvage treatment is still debatable in severe cases.”
Yang et al.
(2021) (3)
Open fractures are frequently occurring orthopaedic emergencies that have been associated with a risk of infection and healing problems, both of the bone and soft tissues (4). These fractures occur due to a wide range of high-energy and lower-energy incidents. High-energy incidents such as motor vehicle and motorcycle accidents and gunshots, as well as lower-energy incidents such as a simple fall from standing or injury playing sport can both lead to open fractures (4) (5). Open fractures are characterized by an open wound or break in the skin near the site of the broken bone (5). This occurs when there is a fragment of bone breaking through the skin at the time of injury (5). Open fractures are different than closed fractures, where there is no open wound. Given this key difference, open fractures require different management strategies compared to closed fractures. Since the skin is broken in open fractures, bacteria can enter the wound easily and cause infection (5). Therefore, infection prevention is prioritized in the early treatment of open fractures (5). The overall management goals include achieving well-aligned bone union, preventing complications, and restoring function (2). While both patient- and treatment-related factors can influence the ultimate outcomes, it has been noted that early management of open fractures may significantly influence long-term outcomes (2). Despite growing evidence-based practice recommendations, there is still a lack of guidance regarding several aspects of open fracture management – including the type of involvement of plastic surgeons across the continuum of care, even though the nature of the injury itself calls for their expertise throughout the diagnosis and treatment process. In this OE Insight, we present the current approaches for the management of open fractures, as well as highlight aspects of an orthoplastic approach that are still defined by controversies and lack of clarity which present meaningful areas of future research.

“A bone infection can be difficult to treat. The patient may require long-term antibiotics and multiple surgical procedures. In extreme cases where the infection cannot be cured and the patient's life is threatened, amputation may even be necessary. For this reason, preventing infection is the focus of early treatment.”
Dunbar & Cannada
(2017) (5)
Overview of Open Fractures
Open fractures are characterized by damage to the soft tissues around the bone, including muscles, tendons, nerves, veins, and arteries and also importantly the periosteum (5). The severity of these fractures depends on the size and number of the fracture fragments, damage to surrounding soft tissues, and the location of the wound and whether soft tissues in that region have good blood supply (5). The settings in which open fractures occur influence the extent of contamination and the greater the damage to bone and soft tissues, the greater the risk of infection (5).

“The management of open fractures presents a challenge due to risk of infection, healing problems and subsequent morbidity. Antibiotics and Tetanus prophylaxis started as soon as possible. Adequate debridement and copious levage remains one of the cornerstones of management of open fractures. Early internal fixation and soft tissue closure is advocated and collaboration with plastic or micro-vascular surgeon early where necessary is advocated. Use of adjuncts to management like vacuum assisted closure, recombinant human bone morphogenic protein 2 may improve tissue and bone healing respectively. The treating surgeon has to adhere to the principles of open fracture management for optimal outcome, prevent complications and decrease hospital stay and costs.”
Buteera & Byimana
(2009) (4)
Managing Open Fractures
Exhibit 1 summarizes the main steps for managing open fractures, adapted from an informational guide published by the American Academy of Orthopaedic Surgeons.
Exhibit 1: Summary of the Management Strategies for Open Fractures (5)
| Stage in Care Continuum | Strategies |
| Initial steps |
|
| Treatment |
|
| Recovery |
|

“The present popular concept of severe open fracture management aims to achieve soft tissue coverage in an early stage. It is based on the collaboration of orthopedic and plastic (microvascular) surgeons in an “orthoplastic” central unit. Compared with the traditional orthopedic approach in which the primary stabilization of the fracture and delayed wound closure are completed in two stages, the combined “orthoplastic” treatment has advantages such as fewer flap failures, lower infection rate, decreased bone-healing time, and short hospital stay.”
Yang et al.
(2021) (3)

“It is well established that the successful treatment of many open fractures involves an ‘orthoplastic’ approach with their primary management being undertaken by both plastic surgeons and orthopaedic surgeons. Godina showed that the successful management of open fractures necessitated immediate debridement and fracture stabilisation with definitive soft tissue cover being undertaken within 72 h. This philosophy has been refined but there is universal agreement that early soft tissue cover is mandatory. Despite this there is virtually no information available about the extent of plastic surgery that is required in the management of open fractures and what little information there is relates only to open fractures of the tibia and ankle.”
Court-Brown et al.
(2015) (6)

“(Among patients who had suffered a severe (Gustilo IIIb or IIIc) open fracture of the tibia after blunt trauma and were treated with radical debridement of the wound outside the zone of injury, skeletal stabilisation and early soft-tissue cover with a vascularised muscle flap), there were four amputations, one early, one mid-term and two late, giving a final rate of limb salvage of 95%. Overall, nine pedicled and 75 free muscle flaps were used; the rate of flap failure was 3.5%. Stabilisation of the fracture was achieved with 19 external and 65 internal fixation devices (nails or plates). Three patients had significant segmental defects and required bone-transport procedures to achieve bony union. Of the rest, 51 fractures (66%) progressed to primary bony union while 26 (34%) required a bone-stimulating procedure to achieve this outcome. Overall, there was a rate of superficial infection of the skin graft of 6%, of deep infection at the site of the fracture of 9.5%, and of serious pin-track infection of 37% in the external fixator group. At final review all patients were walking freely on united fractures with no evidence of infection.”
“External fixation was associated with practical difficulties for the plastic surgeons, a number of chronic pin-track infections and our only cases of malunion. We prefer to use internal fixation.”
Gopal et al.
(2000) (7)
Orthoplastic Management of Open Fractures
While the importance of plastic surgery in managing open fractures is increasingly recognized, there is still limited evidence available to inform the involvement of plastic surgeons across different stages in the care continuum for this type of fracture. In a seminal study by Gopal et al. (2000), a retrospective review of 84 patients with a severe (Gustilo IIIb or IIIc) open fracture of the tibia after blunt trauma between 1990 and 1998, who were treated by a radical debridement of the wound outside the site of injury, skeletal stabilisation and early soft-tissue cover with a vascularised muscle flap by a combined orthopaedic and plastic surgery service, was conducted (7). The overall findings of this study show that a combined orthopaedic and plastic surgical approach for severe open fractures provides good results and is safe. Delay in flap cover longer than 72 hours was associated with the most problems, including acute infection at the skin graft and chronic infection at the fracture site – 14% of patients with a >72 hours delay in flap cover experienced these outcomes. The authors of this study highlighted the importance of referring patients to a specialist centre when possible. In cases where primary transfer is not possible (e.g., in remote geographical areas), the authors recommended an emergency lavage and debridement of the wound, temporary bridging, external fixation and emergency transfer after consulting with the appropriate referral centre.
Since the incipient days of studies examining the value of an orthoplastic approach for managing open fractures, larger epidemiological studies have been conducted to characterize the role of primary plastic surgery in the complete spectrum of these fractures. In a consecutive review of 3297 open fractures between 1988 and 2009, 12.6% of patients were treated with primary plastic surgery, as well as 5.6% treated with split skin grafting and 7.2% with a flap. (6). A greater proportion of patients with open lower limb fractures required primary plastic surgery (27.9%) compared to those with open upper limb fractures (3.5%). Fractures of the femoral diaphysis (25.3%) and those between the proximal tibia and the midfoot (ranging from 24.6% to 44%) required the most primary plastic surgery. The authors of this study noted that the different rates in the use of flaps observed in similar studies can be explained by severity of the fracture – where increased severity necessitated increased use of flaps in fractures of the proximal, diaphyseal and distal tibia and ankle. The authors also highlighted the importance of considering different contextual factors when interpreting prevalence rates of plastic surgery for open fractures from different studies and the time when these surgeries are conducted (i.e. >72 hours) – as these figures will be influenced by whether only trauma centers were included in the studies versus all hospitals and trauma centers in a region, as well as the level of expertise of the surgeons involved in managing open fractures.
With the increase in uptake of an orthoplastic approach for managing open fractures, there has been a growing body of evidence demonstrating the benefits of this approach for improved patient outcomes. Smith et al. (2021) found that in a paediatric population (aged <16 years) with open tibial fractures, a comprehensive and timely approach to orthoplastic care resulted in 100% union, along with no deep infection and flap failures (8). Yang et al. (2021) presented outcomes of patients with severe open fracture (Gustilo IIIb or IIIc) of the limb who underwent a similar radical orthoplastic approach as patients in the Gopal et al. (2000) study (7), which included successful surgical debridement, fixation, and soft tissue reconstruction in one stage (3). In this study, the overall infection rate was 14.6%, which is lower than the results found in previous studies on high-grade open fractures following a two-stage orthopaedic treatment approach (9) (10). Furthermore, the median time to union was 32 weeks, complementing the findings of previous studies that also used a similar orthoplastic approach for treating severe open fractures (11). Additionally, findings of a recent meta-analysis show that an orthoplastic approach decreases time to bone fixation, use of negative pressure wound therapy, and risk of wound/osteomyelitis infections compared to the nonorthoplastic approach for patients with traumatic lower extremity injuries (12).

“The orthoplastic approach proposed by Gopal et al. is relatively radical compared with the “orthoplastic” treatment recommended by the British Orthopaedic Association and the British Association of Plastic Reconstructive and Aesthetic Surgery. The major difference is whether the soft tissue cover is achieved in a single primary procedure. The current popular opinion holds that immediate soft tissue cover is not safe. In contrast, staged surgery for early coverage within 72 h is relatively safe and stable. Nevertheless, Gopal et al. showed excellent union and low rates of infection in aggressive management, proving its effectiveness and operability.”
Yang et al.
(2021) (3)

“Although occasionally a definitive fracture fixation and vascularised soft-tissue cover (‘fix and flap’) may be undertaken safely in the first operation, this may not be pragmatic, nor appropriate, in most centres. Staged surgery allows a period of stabilisation and investigation of the patient in order to plan complex surgery under optimal conditions. For example, it is now understood that a fractured limb with a damaged axial vessel will take longer to unite, and ultimate return of function will be less than that achieved in limbs with normal vasculature. Therefore, we would recommend that prior to surgery, any severe limb injury must have an angiogram by experienced radiologists.”
Khan et al.
(2011) (13)

“Delayed definitive soft tissue coverage is now the accepted choice worldwide, with immediate wound closure the exception. The definition of early versus delayed coverage however, is not a set standard. The urgency of soft tissue cover, especially in grade III injuries suggested by Godina in 1986 [within 72 hours of injury] has been shown to be less required as debridement, antibiotic therapy and wound care has improved. Although the ‘fix and flap’ technique where immediate fracture fixation, debridement and flap coverage has been observed with results not dissimilar to delayed procedures.”
Jordan et al.
(2014) (14)
Notable Controversies of the Orthoplastic Approach
Despite the widespread recognition of the value of an orthoplastic approach for managing open fractures, one of the longest standing areas of opposing recommendations has been the timing of wound coverage. The landmark orthoplastic approach supported by Gopal et al. (2000), which is characterized by a single primary procedure of “fix-and-flap” method, has been described as not pragmatic nor appropriate in many cases (13). Yang et al. (2021) acknowledged that fracture fixation and vascularized soft tissue cover within the first operation is indeed challenging for reconstruction surgeons (3). However, delaying soft tissue cover must be contextualized against the risks associated with this decision. Notably, delayed coverage (even within 72 hours) would be challenging with repeated debridement and has been associated with a higher rate of deep infection (10).
In terms of the technical elements of surgical management of open fracture, there is a lack of evidence supporting some key practices. For example, a 6 hour rule is recommended for performing surgical debridement, although there are studies that show no significant difference in outcomes with delayed debridement (14). Furthermore, there is lack of agreement on the actual amount of tissue that should be excised, with no clear definition of non-viable tissue (14).
There is also lack of consensus on various aspects of postoperative care with an orthoplastic approach. For example, in the United Kingdom, where an orthoplastic approach has been increasingly integrated in their open fracture management strategy in recent years, there are no common guidelines for monitoring flaps across plastic surgery units in this country (15). The most common approach implemented in the UK now involves hourly observations in the first 24 hours, one to two-hourly observations in the next 24 hours, and observations every four hours in the third 24 hour period (15).

“The introduction of a (orthoplastic) collaboration had a significant impact on the in hospital stay. The median time in hospital after acute extremity trauma with soft tissue defects decreased from 68.5 days to 29 days. In the 25 patients after the start of the collaboration, this would correspond to 988 hospital days, and a total cost reduction of 1.170 000 USD. In times where cost-analysis is crucial in public health care, this reduction which corresponds to 70% of one hospital bed/year is obviously beneficial. The reduction of hospital stay may be explained by the decrease in revisions/operations after flap coverage, which may be related to a shorter time to coverage.”
Sommar et al.
(2015) (16)
Current Guidance for Orthoplastic Approach
Notwithstanding that further evidence and guidance is needed to inform multiple aspects of orthoplastic approach for open fracture management, it is clear based on current evidence that this collaborative care model can help improve several patient important outcomes. Even though there is lack of consensus on every aspect of implementing an orthoplastic approach, there are several informational and guidance documents (such as those listed below) that can help surgeons and care facilities determine how to integrate this approach to their practice – a decision that will inevitably be influenced by the resources and expertise available at the local setting.
1. A Review on the Orthoplastic Approach to Lower Limb Reconstruction - https://pubmed.ncbi.nlm.nih.gov/31456609/
2. Setting Up an Effective Orthoplastic Service - https://oxfordmedicine.com/view/10.1093/med/9780198849360.001.0001/med-9780198849360-chapter-20
3. Standards of open lower limb fracture care in the United Kingdom - https://pubmed.ncbi.nlm.nih.gov/33485638/

“(In a systematic review), eight studies evaluated “early” flap coverage, nine studies evaluated “intermediate” flap coverage, and nine studies evaluated “late” flap coverage. Early flap coverage was associated with lower infection rates (p<0.0001) and lower complications (p= 0.15).”
Wood et al.
(2012) (15)
Contributors
References
1. Sop JL, Sop A. Open Fracture Management. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 [cited 2021 Sep 24]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK448083/
2. Miclau T. Open fracture management: Critical issues. OTA International. 2020 Mar;3(1):e074.
3. Yang Z, Xu C, Zhu Y-G, Li J, Wu Z-X, Zou J-W, et al. Radical treatment of severe open fractures of extremities by orthoplastic surgery: a 10-year retrospective study. Journal of Orthopaedic Surgery and Research. 2021 May 27;16(1):340.
4. Buteera AM, Byimana J. Principles of Management of Open Fractures. 2009 Aug 18 [cited 2021 Sep 23]; Available from: https://tspace.library.utoronto.ca/handle/1807/52782
5. Dunbar R, Cannada L. Open Fractures - OrthoInfo - AAOS [Internet]. 2017 [cited 2021 Sep 23]. Available from: https://www.orthoinfo.org/en/diseases--conditions/open-fractures/
6. Court-Brown CM, Honeyman CS, Clement ND, Hamilton SA, McQueen MM. The role of primary plastic surgery in the management of open fractures. Injury. 2015 Dec;46(12):2443–7.
7. Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000 Sep;82(7):959–66.
8. Smith JRA, Fox CE, Wright TC, Khan U, Clarke AM, Monsell FP. Orthoplastic management of open tibial fractures in children : a consecutive five-year series from a paediatric major trauma centre. Bone Joint J. 2021 Jun;103-B(6):1160–7.
9. Mathews JA, Ward J, Chapman TW, Khan UM, Kelly MB. Single-stage orthoplastic reconstruction of Gustilo–Anderson Grade III open tibial fractures greatly reduces infection rates. Injury. 2015 Nov 1;46(11):2263–6.
10. Hull PD, Johnson SC, Stephen DJG, Kreder HJ, Jenkinson RJ. Delayed debridement of severe open fractures is associated with a higher rate of deep infection. Bone Joint J. 2014 Mar;96-B(3):379–84.
11. Boriani F, Haq AU, Baldini T, Urso R, Granchi D, Baldini N, et al. Orthoplastic surgical collaboration is required to optimise the treatment of severe limb injuries: A multi-centre, prospective cohort study. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2017 Jun 1;70(6):715–22.
12. Klifto KM, Azoury SC, Othman S, Klifto CS, Levin LS, Kovach SJ. The Value of an Orthoplastic Approach to Management of Lower Extremity Trauma: Systematic Review and Meta-analysis. Plastic and Reconstructive Surgery – Global Open. 2021 Mar;9(3):e3494.
13. Khan U, Kelly MB, Pleat J, Chesser TJS. Orthoplastics: an integral evolution within comprehensive trauma care. Injury. 2011 Oct;42(10):969–71.
14. Jordan DJ, Malahias M, Khan W, Hindocha S. The Ortho-Plastic Approach to Soft Tissue Management in Trauma. The Open Orthopaedics Journal [Internet]. 2014 Oct 31 [cited 2021 Sep 29];8(1). Available from: https://www.openorthopaedicsjournal.com/VOLUME/8/PAGE/399/FULLTEXT/
15. Loh B, Lim JA, Seah M, Khan W. Perioperative management of open fractures in the lower limb. J Perioper Pract. 2021 Jul 2;17504589211012150.
16. Sommar P, Granberg Y, Halle M, Skogh A-CD, Lundgren KT, Jansson K-Å. Effects of a formalized collaboration between plastic and orthopedic surgeons in severe extremity trauma patients; a retrospective study. J Trauma Manag Outcomes. 2015 Apr 15;9:3.
© OrthoEvidence Inc. All Rights Reserved.




 LOGIN
LOGIN


