HIGHLIGHTS
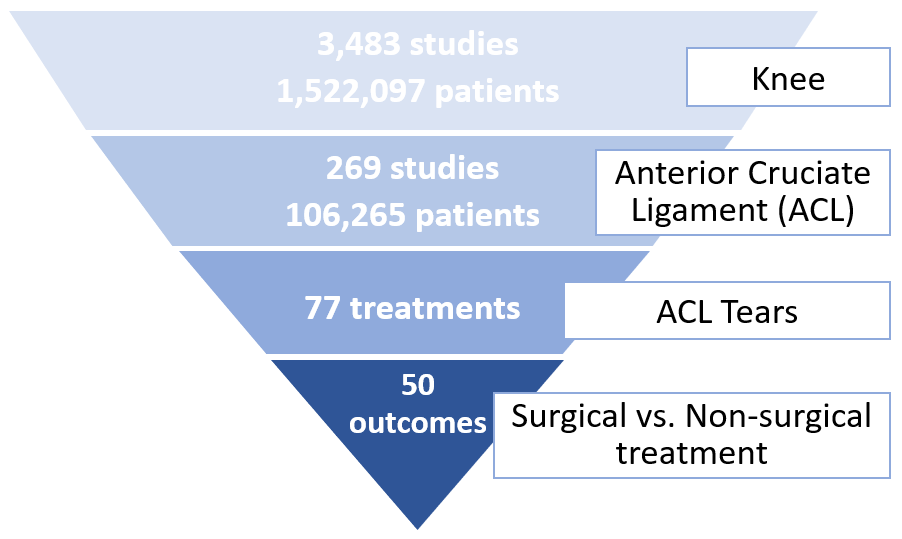
- With the updated search by October 2021, OE M.I.N.D. contains data from nearly 3,500 RCTs related to knee conditions with over 1,500,000 patients.
- For patients with anterior cruciate ligament (ACL) injury, early reconstruction was associated with superior outcomes in Tegner activity score, stability, re-injury and revision surgery compared to rehabilitation alone either up to 2 years or longer than 2 years’ follow-up.
- There was no significant difference between surgical and non-surgical treatment in composite clinical outcomes, pain, and incidence of return to preinjury activity level during follow-up periods of either up to 2 years or 2 to 15 years post treatment.
- In terms of either reconstruction or rehabilitation for ACL injury, a total of 45 studies were found to be currently ongoing around the world, aiming to recruit over 12,000 patients based on data from clinicaltrials.gov.
- Since 2005, the manufacturers that have published the most research associated with reconstruction for ACL are Smith & Nephew, Arthrex, Ethicon, DePuy Synthes, Stryker and Johnson & Johnson.
Anterior cruciate ligament (ACL) injury is a common orthopaedic condition that affects knee joint stability and is associated with time lost from sport and an increased risk of osteoarthritis (Hewett et al., 2006; Lien-Iversen et al., 2020). Studies reported an annual incidence between 0.15% and 3.7% of ACL injuries among professional athletes and the incidence has been increasing (Moses et al., 2012; Secrist et al., 2016).
Treatment of ACL injury includes both surgical reconstruction and non-surgical options of rehabilitation, bracing and activity modification (Bogunovic & Matava, 2013). Over 130,000 ACL reconstructions were performed in the United States in 2006, and the rate is increasing (Buller et al., 2014). Whether there is difference in patient outcomes between the surgical and non-surgical treatment for ACL injury is a critical question to guide clinical decision.
In this OE Original, we present analytics using OE M.I.N.D. that include a scoping review of published studies, meta-analysis results and quality of evidence, cumulative evidence synthesized by time and a profile of ongoing trials for surgical versus non-surgical treatment for ACL injury. All of the data were extracted from randomized controlled trials (RCTs) by experienced medical literature reviewers. OE M.I.N.D. updates the data on a daily basis, with new trials and data being constantly added. The results in this OE Original were based on analyses performed on October 25, 2021.
1. OE M.I.N.D. Meta Analyzer --- Overview of the available evidence
Over one and half million patients across nearly 3,500 studies were reported for knee conditions. Of these, over 106,000 patients across 269 studies examined ACL conditions. There are 77 treatments that were studied for ACL tears, and 50 outcome measures were reported evaluating the effectiveness and safety of surgical versus non-surgical treatment (Figure 1).
Figure 1. Summary of research topic according to anatomical region, condition and treatment
2. OE M.I.N.D. Meta Analyzer --- Effectiveness of treatments
We identified 6 articles that reported 5 RCTs with 577 patients that compared surgical treatment with non-surgical treatment for patients with ACL tears. The surgical treatment in all the studies was ACL reconstruction plus rehabilitation and the non-surgical treatment was rehabilitation alone or application of a cast (Frobell et al., 2010 & 2013; Meunier et al., 2007; Reijman et al., 2021; Sandberg et al., 1987; Tsoukas et al., 2016). For studies in which non-surgical patients were allowed to undergo a delayed ACL reconstruction, we analyzed outcomes of patients who had rehabilitation alone as they were reported separately in those studies (Frobell et al., 2010 & 2013; Reijman et al., 2021). All the included RCTs followed up with patients for 2 to 15 years. The characteristics of the RCTs included in meta-analysis are presented in Table 1.
Table 1. Characteristics of RCTs included in meta-analysis | |||||
Author, Year | Country | Number of patients | Patients | Surgical group | Non-surgical group |
Frobell et al., 2010 & 2013 | Sweden | 121 | Patients with ACL injury within 4 weeks | Structured rehabilitation and ACL reconstruction surgery performed within 10 weeks after the injury; procedure chosen by surgeons’ preferences: patella-tendon (N=25) or hamstring-tendon (N=36). | Structured rehabilitation with elective delayed reconstruction; 23 patients (39%) underwent ACL reconstruction in 2 years of follow-up. |
Meunier et al., 2007 | Sweden | 100 | Patients with an acute and total rupture of the ACL, age =< 30 years | ACL reconstruction with (N=32) and without (N=10) augmentation, using a technique described by Andersson with multiple sutures. Postoperative rehabilitation. | Rehabilitation alone |
Reijman et al., 2021 | Netherlands | 167 | Patients with a complete primary ACL rupture within 2 months | Arthroscopic ACL reconstruction; technique and graft chosen by surgeons’ preferences; the majority of patients had a hamstring graft. Postoperative rehabilitation. | A minimum of three months of rehabilitation with elective delayed reconstruction; 41 patients (50%) underwent ACL reconstruction in 2 years of follow-up, at an average of 10.6 months after randomization. |
Sandberg et al., 1987 | Sweden | 157 | Patients who had injuries to the ACL or both ACL and MCL within 2 weeks | Immediate suture of ligaments without augmentation by other tissue with modified Palmer’s technique. Casts were applied postoperatively. | Application of a plaster cast for 6 weeks, and isometric exercises. |
Tsoukas et al., 2016 | The United Kingdom/Greece | 32 | Patients with isolated ACL injuries, BMI < 30 | Arthroscopic ACL reconstruction, four-stranded semitendinosus-gracilis tendon autografts. Postoperative rehabilitation. | Rehabilitation alone |
Note: ACL, anterior cruciate ligament; MCL, medial collateral ligament.
We are presenting the meta-analysis results of composite clinical outcomes, pain, Tegner activity score, incidence of returning to preinjury activity level and the stability outcomes during two time frames of follow-up: up to 2 years, and beyond 2 years post treatment. For incidence of re-injury and revision surgery, we are presenting their overall results at the longest follow-up.
2.1 Composite clinical outcomes (0 to 100, a higher score indicates better recovery)
Lysholm knee score, International Knee Documentation Committee (IKDC) score and Knee Injury and Osteoarthritis Outcome Score (KOOS) symptoms subscale are normalized on a 0 to 100 scale to assess patient recovery (Collins et al., 2011; Velentgas et al., 2010).
In the comparison of ACL reconstruction versus rehabilitation alone for the composite clinical outcomes, a total of 620 patients from 5 studies published between 1987 to 2021 are included in the analysis. There was no significant difference in the composite clinical outcomes between the two treatments up to 2 years [mean difference (MD), 1.69; 95% confidence interval (CI), -0.76 to 4.14 points] or beyond 2 years follow-up (MD, -1.93; 95% CI, -5.05 to 1.19 points). The certainty of the evidence by GRADE assessment was rated as very low due to serious risk of bias, inconsistency and imprecision (Figure 2).
Figure 2. Forest plot of composite clinical outcomes on a 0-100 scale
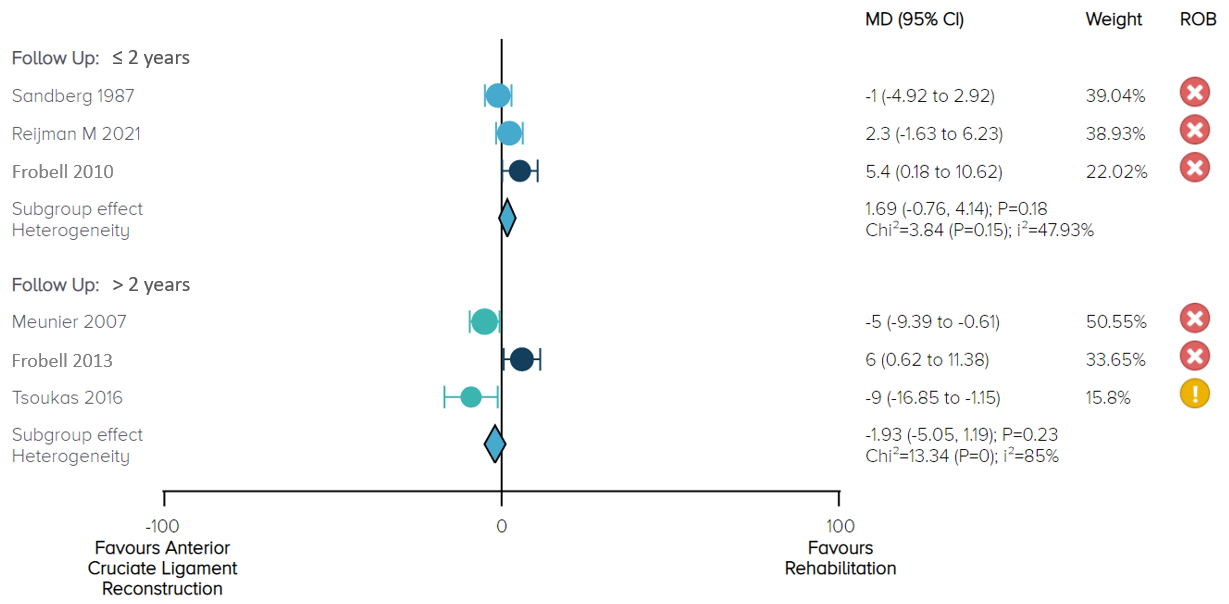
Notes: ROB = risk of bias; red circle with a cross mark = high risk of bias; yellow circle with an exclamation mark = have some concerns.
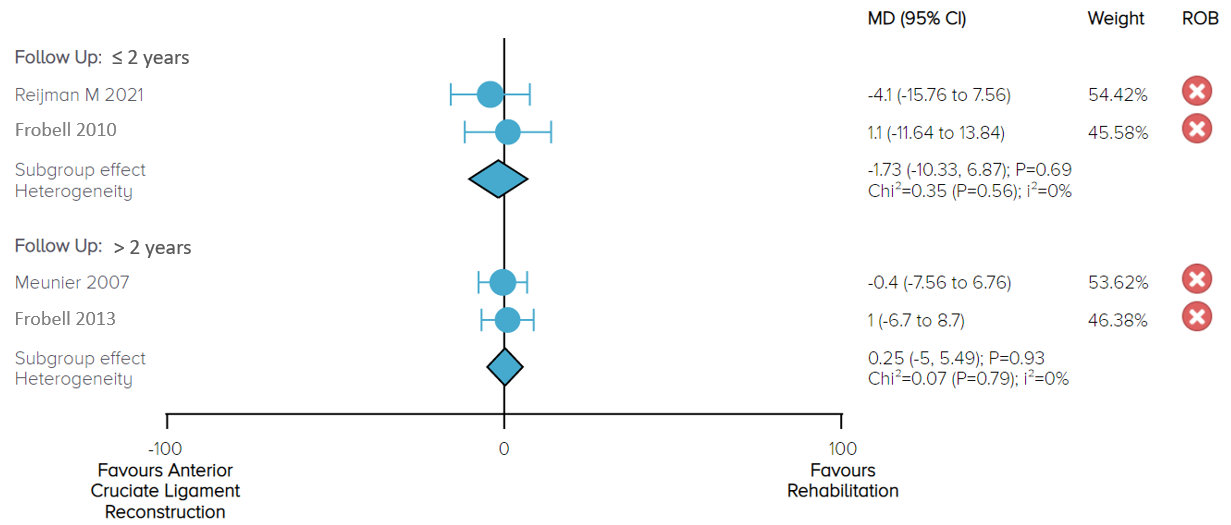
2.2 Pain score (0 to 100, a higher score indicates worse pain)
Three studies including 388 patients reported numeric rating scale or KOOS pain score up to 15 years follow-up. There was no significant difference in pain between ACL reconstruction and rehabilitation alone up to 2 years (MD, -1.73; 95% CI, -10.33 to 6.87 points) or beyond 2 years follow-up (MD, 0.25; 95% CI, -5 to 5.49 points). We rated the certainty of evidence as low due to serious risk of bias and imprecision (Figure 3).
Figure 3. Forest plot of pain on 0-100 score
2.3 Tegner activity score (0 to 10, a higher score indicates higher level of activity)
A total of 253 patients from 3 RCTs reported Tegner activity scores at 2 and 5 years (Frobell et al., 2010 & 2013), 10 years (Tsoukas et al., 2016) and 15 years (Meunier et al., 2007) follow-up. Up to 2 years post treatment, the effect demonstrates that compared to rehabilitation alone, ACL reconstruction results in a significant improvement in activity with patients experiencing, on average, a 1.5 (95% CI, 0.87 to 2.13) points improvement. Beyond 2 years post treatment, the overall effect demonstrates that ACL reconstruction results in a significant improvement in activity with patients experiencing, on average, a 0.96 (95% CI, 0.64 to 1.29) point improvement. Nevertheless, the effects and 95% CI in both follow-up durations do not exceed the recommended minimum detectable change of 1 point on the 0 to 10 Tegner activity scale (Briggs et al., 2009; Copay et al., 2018) (Figure 4).
Figure 4. Forest plot of Tegner activity score on a 0-10 scale
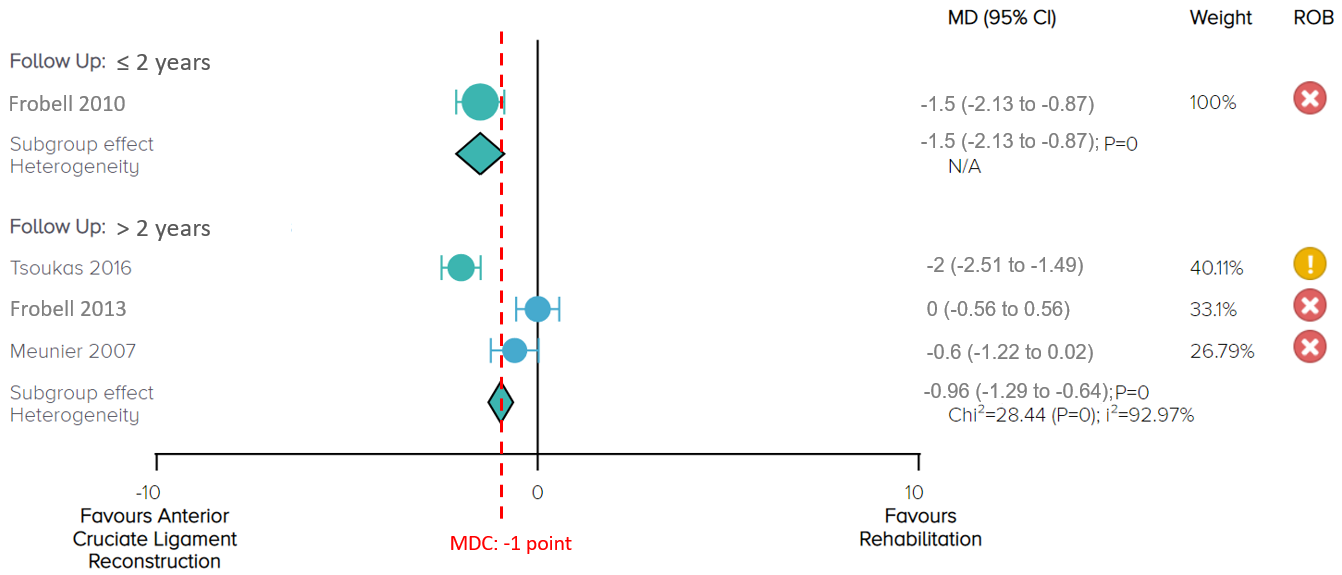
Notes: MDC = minimum detectable change; ROB = risk of bias; red circle with a cross mark = high risk of bias; yellow circle with an exclamation mark = have some concerns.
2.4 Incidence of returning to preinjury activity level
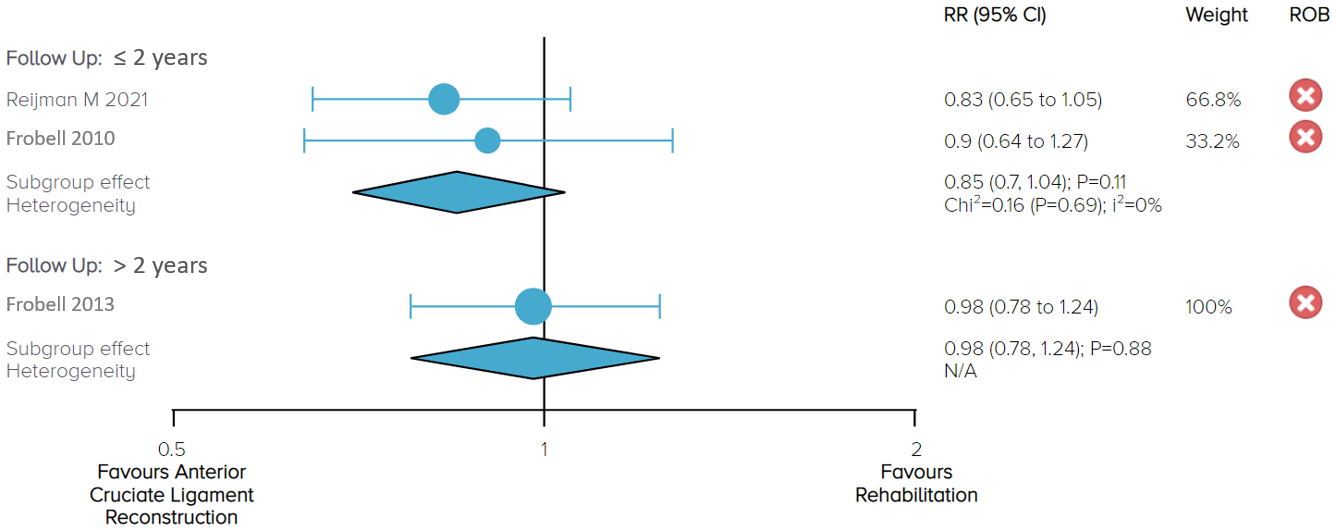
In the comparison of ACL reconstruction versus rehabilitation alone for the outcome of returning to the same activity level before the injury, a total of 288 patients from 2 studies published between 2010 to 2021 are included in the analysis. There was no significant difference in incidence of returning to preinjury activity level between the two treatments =< 2 years [relative risk (RR), 0.85; 95% CI, 0.7 to 1.04] and beyond 2 years (RR, 0.98; 95% CI, 0.78 to 1.24), with low certainty of evidence. To note, the statistical difference is at borderline significance as the lower bound of the 95% CI is close to the RR of 1 for the outcome =< 2 years post treatment (Figure 5).
Figure 5. Forest plot of returning to preinjury activity level
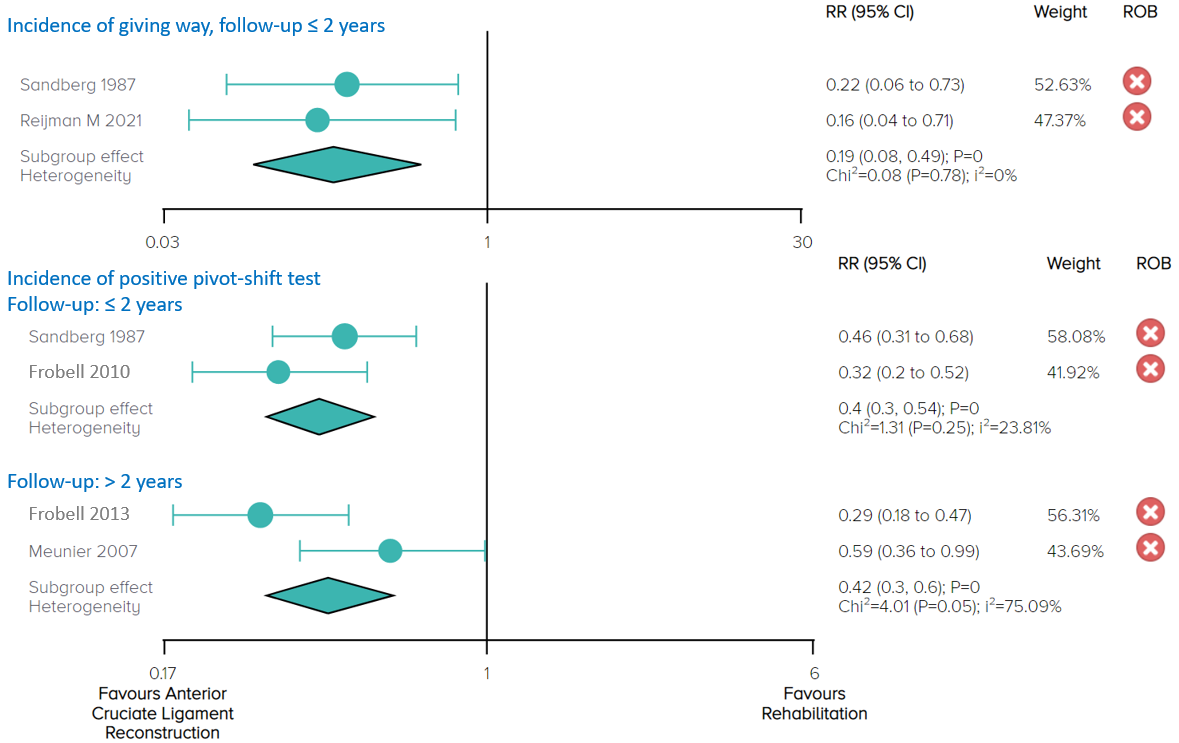
2.5 Stability (Incidence of giving way; Incidence of positive pivot-shift test)
Two studies including 367 patients reported incidence of giving way up to 2 years follow-up. The overall effect demonstrates that the risk of giving way is significantly lower with ACL reconstruction than with rehabilitation alone (RR, 0.19; 95% CI, 0.08 to 0.49), with moderate certainty of evidence (Figure 6).
Three studies including 421 patients reported incidence of positive results in the pivot-shift test. The overall effect demonstrates that the risk of positive pivot-shift test is significantly lower with ACL reconstruction than with rehabilitation alone up to 2 years follow-up (RR, 0.4; 95% CI, 0.3 to 0.54, moderate certainty of evidence) as well as during follow-up beyond 2 years (RR, 0.42; 95% CI, 0.3 to 0.6, low certainty of evidence) (Figure 6).
Figure 6. Forest plot of giving way and positive pivot-shift test (Stability)
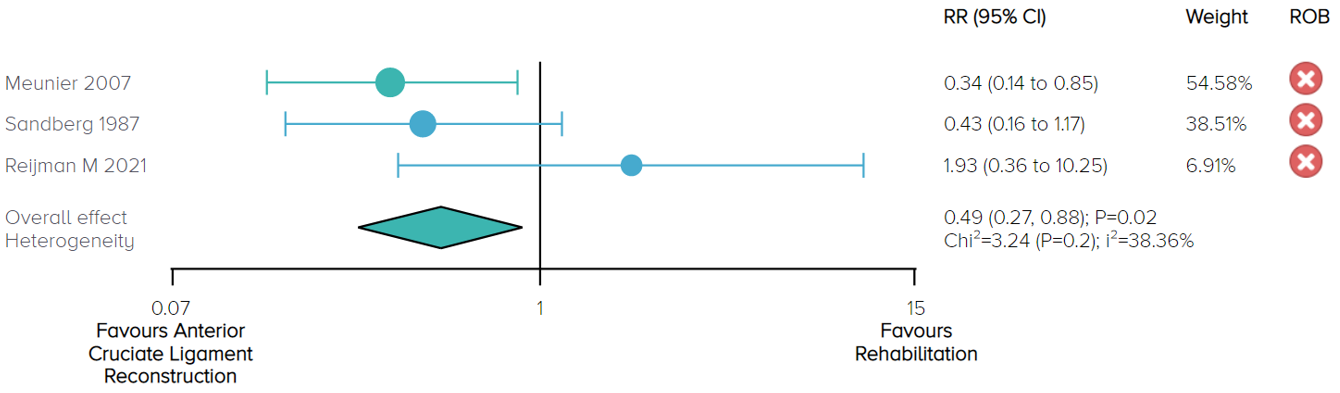
2.6 Incidence of re-injury
In the comparison of ACL reconstruction versus rehabilitation alone for the outcome of re-injury at the longest follow-up (2 to 15 years), a total of 467 patients from 3 studies published between 1987 to 2021 are included in the analysis. One study favours ACL reconstruction and 2 studies show no difference between the two treatments. The overall effect demonstrates that the risk of re-injury is significantly lower with ACL reconstruction than with rehabilitation [RR, 0.49; 95% CI, 0.27 to 0.88], with moderate certainty of evidence (Figure 7).
Figure 7. Forest plot of incidence of re-injury
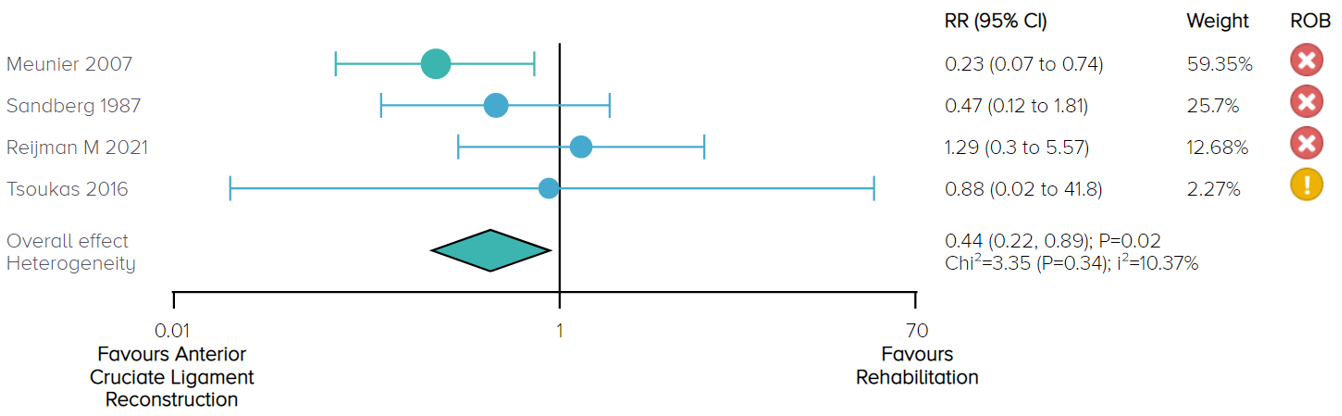
2.7 Incidence of revision surgery
In the comparison of ACL reconstruction versus rehabilitation alone for the outcome of revision surgery at the longest follow-up (2 to 15 years), a total of 499 patients from 4 studies published between 1987 to 2021 are included in the analysis. One study favours ACL reconstruction and 3 studies show no difference between the two treatments. The overall effect demonstrates that the risk of revision surgery is significantly lower with ACL reconstruction than with rehabilitation [RR, 0.44; 95% CI, 0.22 to 0.89], with moderate certainty of evidence (Figure 7).
Figure 8. Forest plot of incidence of revision surgery
We present a summary of the eight outcome measures in Table 2.
Table 2. Summary and certainty of the evidence
Outcome | =< 2 years | > 2 years to 15 years |
Composite clinical outcomes | No difference (Very low certainty) | No difference (Very low certainty) |
Pain | No difference (Low certainty) | No difference (Low certainty) |
Tegner activity score | Favours ACL reconstruction (Low certainty) | Favours ACL reconstruction (Very low certainty) |
Returning to preinjury activity level | No difference (Low certainty) | No difference (Low certainty) |
Stability (Incidence of giving way) | Favours ACL reconstruction (Moderate certainty) | -- |
Stability (Incidence of positive pivot-shift test) | Favours ACL reconstruction (Moderate certainty) | Favours ACL reconstruction (Low certainty) |
Re-injury at the longest follow-up | Favours ACL reconstruction (Moderate certainty) | |
Revision surgery at the longest follow-up | Favours ACL reconstruction (Moderate certainty) | |
Note: ACL, anterior cruciate ligament.
3. OE M.I.N.D. Forecaster --- Sequential meta-analysis
The trends in treatment effects over time show that, when new RCTs are reported and more patients are included in the analysis, precision of effects increases for all the outcomes at their longest follow-up (narrower 95% CI over time) (Figures 9-11).
There is no significant difference between ACL reconstruction and rehabilitation for patients who had ACL injuries in terms of composite clinical outcomes (normalized scale of Lysholm knee score, IKDC score and KOOS symptoms) and pain, and the findings have remained consistent (Figure 9).
Figure 9. Sequential meta-analysis result for composite clinical outcomes and pain
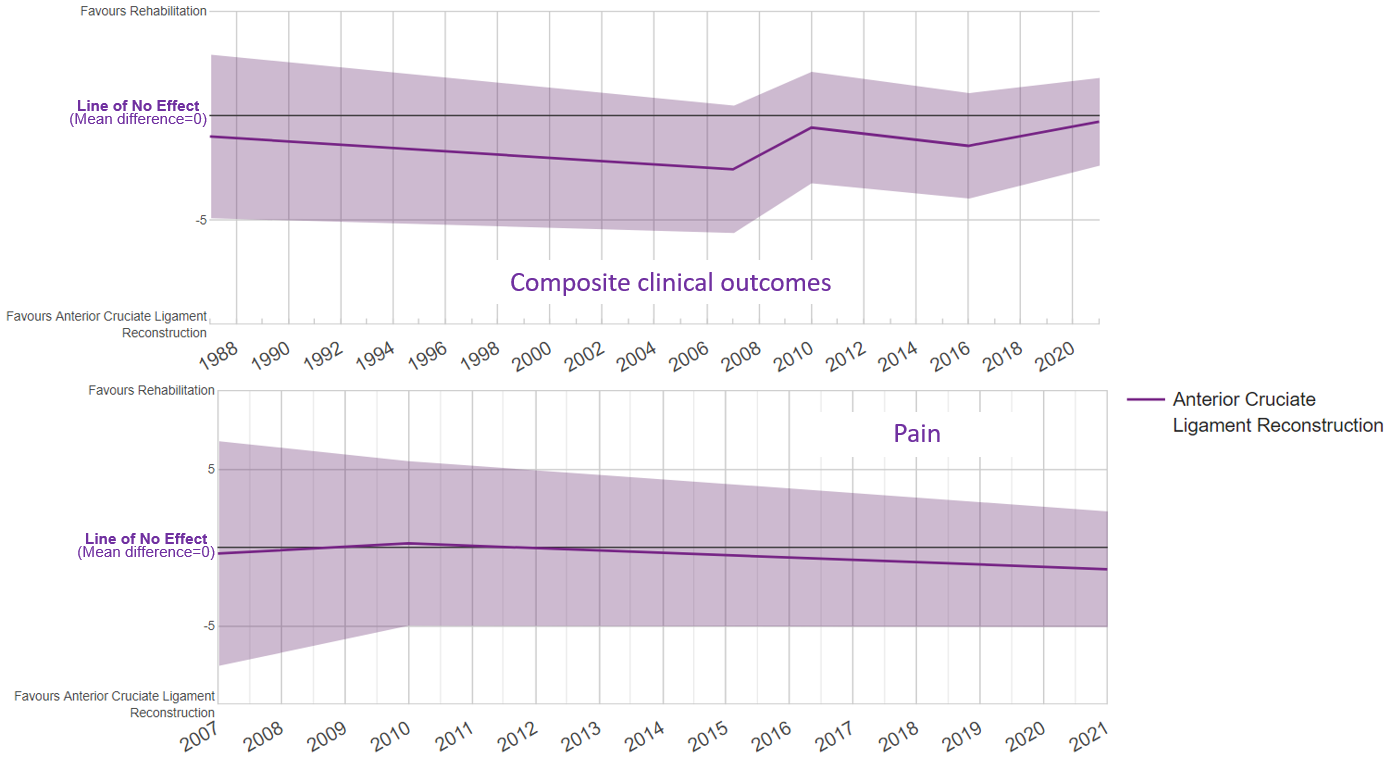
For Tegner activity score, the treatment effect started with the first reported study with no significant difference between ACL reconstruction and rehabilitation alone. After examining all of the evidence over time, the final treatment effect favoured ACL reconstruction, and the final effect and 95% CI exceeded the recommended MDC (Figure 10).
There is no significant difference between ACL reconstruction and rehabilitation for incidence of return to preinjury activity level and the findings have remained consistent (Figure 10).
Figure 10. Sequential meta-analysis result for Tegner activity score, and return to preinjury activity level
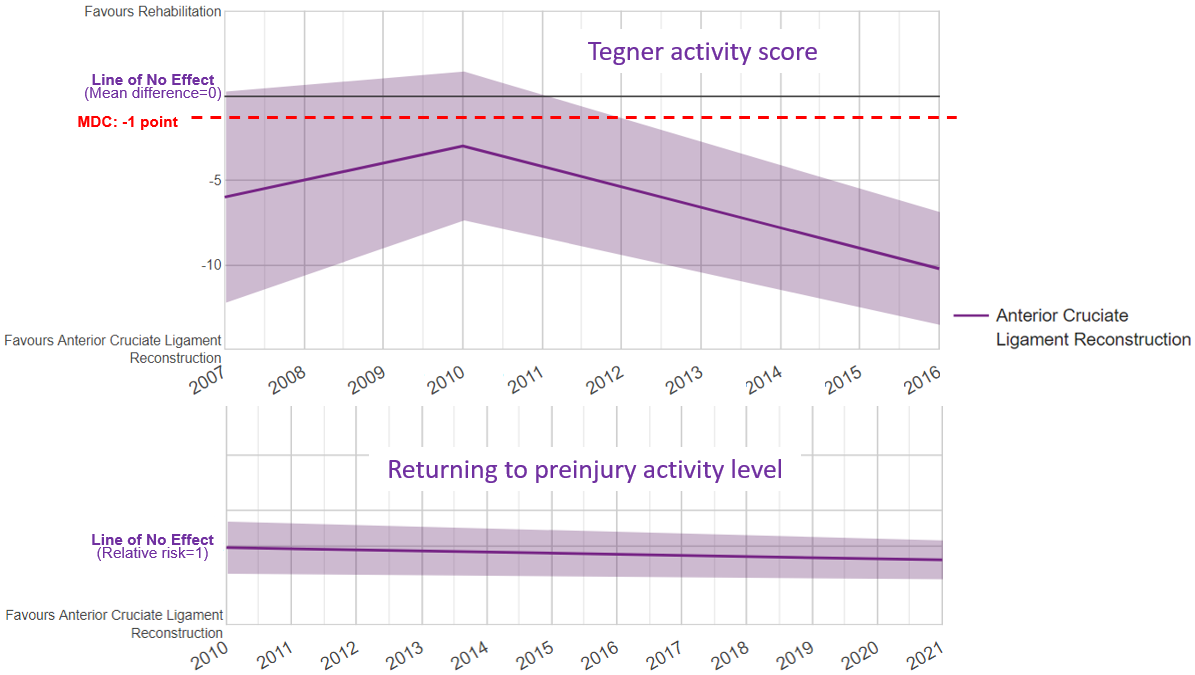
For both incidence of giving way and incidence of positive pivot-shift test that indicate stability outcome, the overall effects favours ACL reconstruction compared to rehabilitation alone, and the findings have remained consistent (Figure 11).
In terms of incidence of re-injury and incidence of revision surgery, the treatment effect started with the first reported study with no significant difference between the two treatments. After examining all of the evidence over time, the final treatment effect favoured ACL reconstruction (Figure 11).
Figure 11. Sequential meta-analysis result for incidence of giving way, positive result in pivot-shift test, re-injury and revision surgery
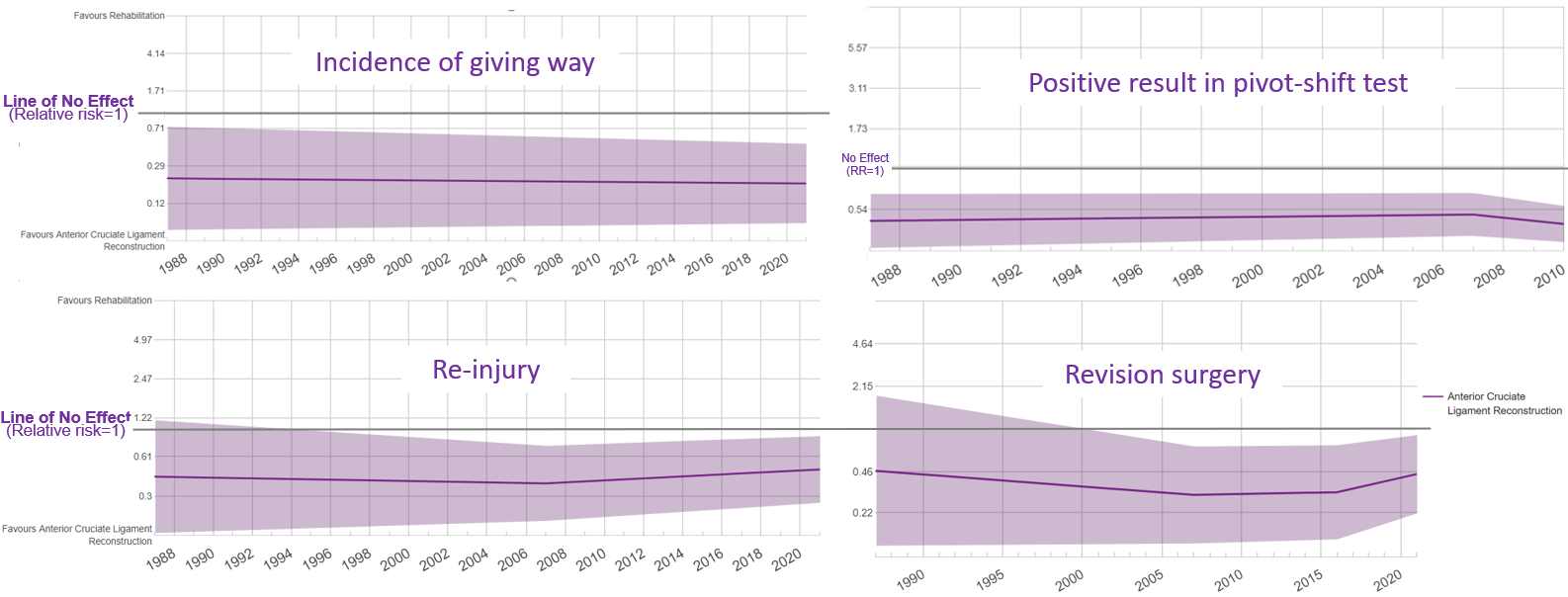
4. OE M.I.N.D Ongoing trials report
For intervention comparisons that include either ACL reconstruction or rehabilitation, a total of 45 studies were found to be currently ongoing around the world, aiming to recruit 12,798 patients. Eleven of these 45 ongoing studies (24.4%) are being conducted in the United States. Forty-two of them (93.3%) are interventional studies. (Figure 12).
Figure 12. Ongoing trials of ACL reconstruction or rehabilitation for ACL injury
5. OE M.I.N.D. Research Planning Tool
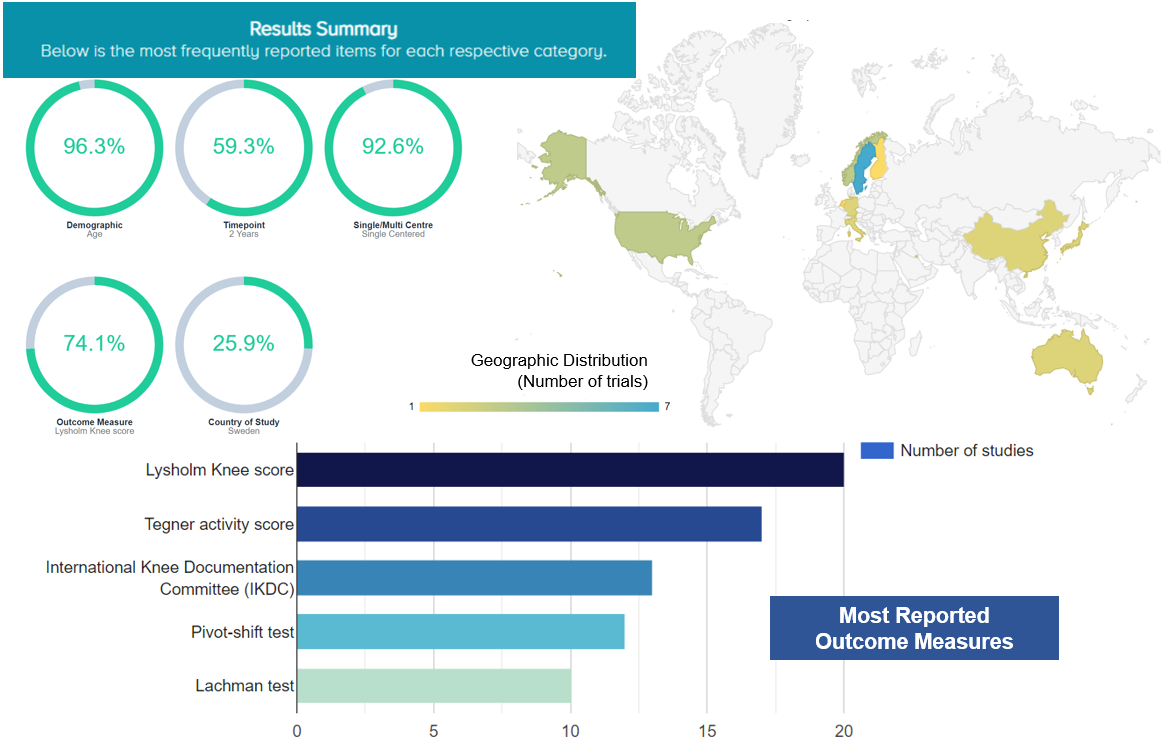
The OE M.I.N.D. Research Planning Tool provides us with an overview of characteristics of prior RCTs. For studies investigating effects of reconstruction for ACL injury, the most frequently reported characteristics include: patient demographics, age (96.3% studies reported age); follow-up time point, 2 years (59.3% studies reported outcomes at 2 years’ follow-up); studies conducted at a single center (92.6%); Lysholm Knee Score (74.1%); and the country, Sweden (25.9%) (Figure 13).
Figure 13. The most frequently reported characteristics of studies investigating effects of ACL reconstruction for ACL injury
6. OE MIND Academic market analysis --- Top sponsors
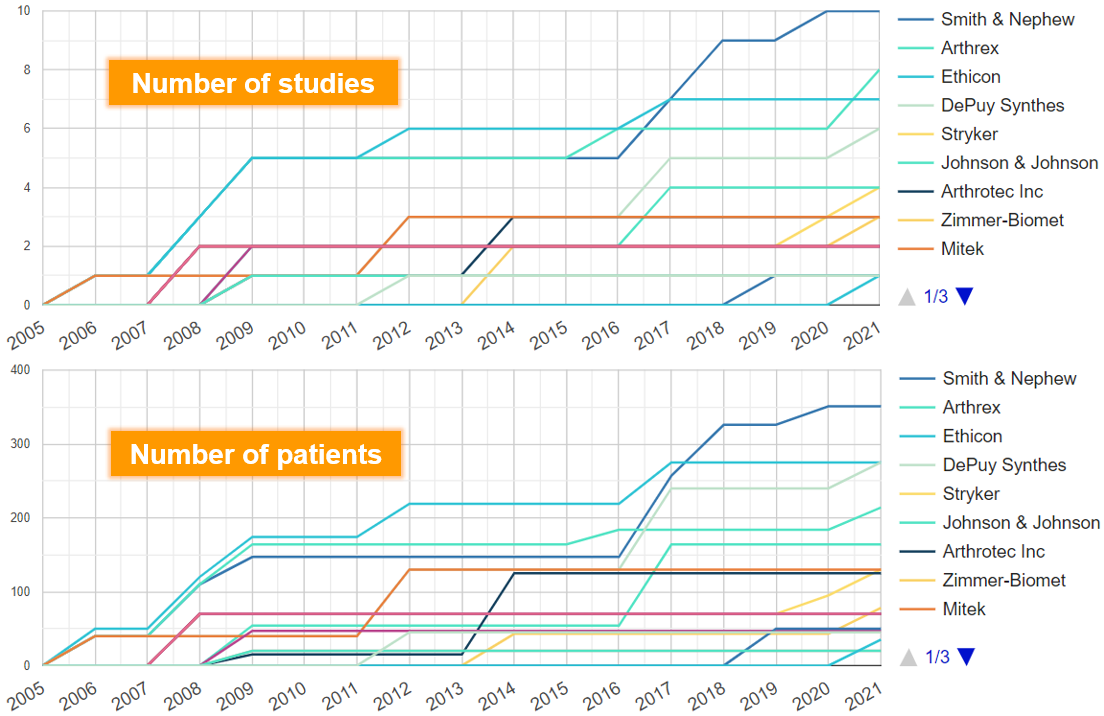
For investigating effects of reconstruction for ACL injury, we found that since 2005, the manufacturers that have published the most research are Smith & Nephew (N of studies=10), Arthrex (N=8), Ethicon (N=7), DePuy Synthes (N=6), Stryker (N=4) and Johnson & Johnson (N=4) (Figure 14).
The manufacturers with the largest cumulative sample size are Smith & Nephew (N of patients=351), Ethicon (N=275), DePuy Synthes (N=275), Arthrex (N=214) and Johnson & Johnson (N=164) (Figure 14).
Figure 14. Manufacturers with most researches for ACL reconstruction
Discussion
In this OE Original, we identified 5 RCTs that compared the efficacy of ACL reconstruction versus rehabilitation alone for patients with ACL injury. In the meta-analysis, evidence of low to very low quality showed that there was no significant difference between the two treatments in composite clinical outcomes (normalized scale of Lysholm knee score, IKDC score and KOOS symptoms), pain score, and incidence of return to preinjury activity level during follow-up periods of either =< 2 years or > 2 to 15 years. These findings are consistent with the results from previously published systematic reviews that found no difference in patient reported measures (Blom et al., 2021; Monk et al., 2016).
For the Tegner activity score, the overall effect favoured ACL reconstruction in both shorter (=< 2 years) and longer (> 2 to 15 years) follow-up periods. The quality of evidence in both follow-up periods was rated to be low due to risk of bias and imprecision and very low due to risk of bias, imprecision and inconsistency, accordingly (refer to introduction of GRADE at https://myorthoevidence.com/Blog/Show/32). The effects and 95% CI in Tegner activity score in both shorter and longer follow-up periods demonstrated statistical significance but did not exceed the minimum detectable change.
In terms of knee joint stability (incidence of giving way and incidence of positive result in pivot-shift test), re-injury and revision surgery, moderate or low quality of evidence showed results favouring ACL reconstruction compared to rehabilitation alone.
We did not find available data from the included RCTs to conduct a subgroup analysis by different severities of ACL injury. The serious risk of bias due to lack of blinding to clinicians and patients was one of the major concerns during the evidence quality assessment (Guyatt et al., 2011).
The choice of surgical or non-surgical treatment for ACL injury may depend on a patient’s age, gender, role in professional sports and desired level of activity after recovery (Bogunovic & Matava, 2013). Surgical procedure is recommended for individuals who desire to continue the IKDC Activity Level I and II like jumping, cutting sports, high-risk pivoting sports, side-to-side sports and heavy manual work; whilst non-surgical treatment is recommended for individuals whose usual activity falls in Level III and IV activities like light manual work, noncutting sports and sedentary activities (Nebelung & Wuschech, 2005; Daniel & Fithian, 1994; Bogunovic & Matava, 2013). The findings of our meta-analyses may serve as supporting evidence to the recommendation.
Additional future studies with larger sample sizes and with at least 2 years follow-up are valuable to evaluate the clinical outcomes including function, pain and returning to activity before injury, and associated cost.
Bottom line
Meta-analysis of 5 RCTs showed that for patients with ACL injury, ACL reconstruction was associated with a small effect in Tegner activity score, significantly superior stability outcomes, lower risk of re-injury and lower risk of revision surgery, compared to rehabilitation alone in follow-up periods of =< 2 years and > 2 to 15 years. No significant difference was found between the two treatments in outcomes of composite clinical outcomes, pain, and incidence of return to preinjury level.
Reference
Blom AW, Donovan RL, Beswick AD, Whitehouse MR, Kunutsor SK. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence. bmj. 2021 Jul 8;374.
Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-PS), knee outcome survey activities of daily living scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis care & research. 2011 Nov;63(S11):S208-28.
Bogunovic L, Matava MJ. Operative and nonoperative treatment options for ACL tears in the adult patient: a conceptual review. The Physician and sportsmedicine. 2013 Nov 1;41(4):33-40.
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. The American journal of sports medicine. 2009 May;37(5):890-7.
Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthopaedic journal of sports medicine. 2014 Dec 26;3(1):2325967114563664.
Copay AG, Eyberg B, Chung AS, Zurcher KS, Chutkan N, Spangehl MJ. Minimum clinically important difference: current trends in the orthopaedic literature, part II: lower extremity: a systematic review. JBJS reviews. 2018 Sep 1;6(9):e2.
Daniel DM, Fithian DC. Indications for ACL surgery. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1994 Aug 1;10(4):434-41.
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. New England Journal of Medicine. 2010 Jul 22;363(4):331-42.
Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Bmj. 2013 Jan 24;346.
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). Journal of clinical epidemiology. 2011 Apr 1;64(4):407-15.
Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. The American journal of sports medicine. 2006 Feb;34(2):299-311.
Lien-Iversen T, Morgan DB, Jensen C, Risberg MA, Engebretsen L, Viberg B. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? A systematic review and meta-analysis. British journal of sports medicine. 2020 May 1;54(10):592-8.
Meunier A, Odensten M, Good L. Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: A randomized study with a 15-year follow-up. Scandinavian journal of medicine & science in sports. 2007 Jun;17(3):230-7.
Monk AP, Davies LJ, Hopewell S, Harris K, Beard DJ, Price AJ. Surgical versus conservative interventions for treating anterior cruciate ligament injuries. Cochrane Database of Systematic Reviews. 2016(4).
Moses B, Orchard J, Orchard J. Systematic review: annual incidence of ACL injury and surgery in various populations. Research in Sports Medicine. 2012 Jul 1;20(3-4):157-79.
Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament—deficient knees in high-level athletes. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2005 Jun 1;21(6):696-702.
Reijman M, Eggerding V, van Es E, van Arkel E, van den Brand I, van Linge J, Zijl J, Waarsing E, Bierma-Zeinstra S, Meuffels D. Early surgical reconstruction versus rehabilitation with elective delayed reconstruction for patients with anterior cruciate ligament rupture: COMPARE randomised controlled trial. bmj. 2021 Mar 9;372.
Sandberg R, Balkfors B, Nilsson B, Westlin N. Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. The Journal of bone and joint surgery. American volume. 1987 Oct 1;69(8):1120-6.
Secrist ES, Frederick RW, Tjoumakaris FP, Stache SA, Hammoud S, Freedman KB. A comparison of operative and nonoperative treatment of anterior cruciate ligament injuries. JBJS reviews. 2016 Nov 1;4(11).
Tsoukas D, Fotopoulos V, Basdekis G, Makridis KG. No difference in osteoarthritis after surgical and non-surgical treatment of ACL-injured knees after 10 years. Knee Surgery, Sports Traumatology, Arthroscopy. 2016 Sep;24(9):2953-9.
Velentgas P, Dreyer NA, Wu AW. Outcome Definition and Measurement. In: Velentgas P, Dreyer NA, Nourjah P, et al., editors. Developing a Protocol for Observational Comparative Effectiveness Research: A User's Guide. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Jan. Chapter 6. Available from: https://www.ncbi.nlm.nih.gov/books/NBK126186/




 LOGIN
LOGIN


Join the Conversation
Please Login or Join to leave comments.
Orthopaedic Surgeon - Canada
This is quite a Mind-Bender. My conclusion, which I am prepared to be corrected upon, is that we need much more detailed assessment tools to come up with the most effective treatment plan for each individual patient rather than "with me they all get reconstruction" or " none get reconstruction". But I was not enabled sufficiently with the reports to reconcile that decision process.
Other - United States
I am probably not the typical user of this site. I'm actually a patient that experienced a grade 3 tear of the ACL a month ago. I am 42 and my doctor leaned towards recommending that I have no surgery. I agreed with him, and have since been researching studies on nonsurgical solutions for ACL tears. This summary of the various ACL studies is illuminating. There appears to be no distinct benefit to surgery for someone like me, since I do not play sports. My primary concern is the development of osteoarthritis, which appears to happen in patients regardless of the treatment option they pursue (surgery vs no surgery). I would like to see a study on ways to reduce the risk of developing osteoarthritis for nonoperative patients and also whether stem cells can help someone with a grade 3 tear.
Orthopaedic Surgeon - Canada
Unfortunately these studies don't seem to address the question as to WHO should have an ACL reconstruction. A 20 yo is very different from a 45yo. A competitive soccer player is very different from a competitive biker who is very different from a downhill skiier from a recreational hockey player. I wish the studies started to tease out those differences to give us more meaningful studies to draw information from.