Addition of Dexmedetomidine, a Sedative-analgesic Agent, to Femoral Nerve Block for Total Knee Arthroplasty: A Systematic Review of Randomized Controlled Trials .
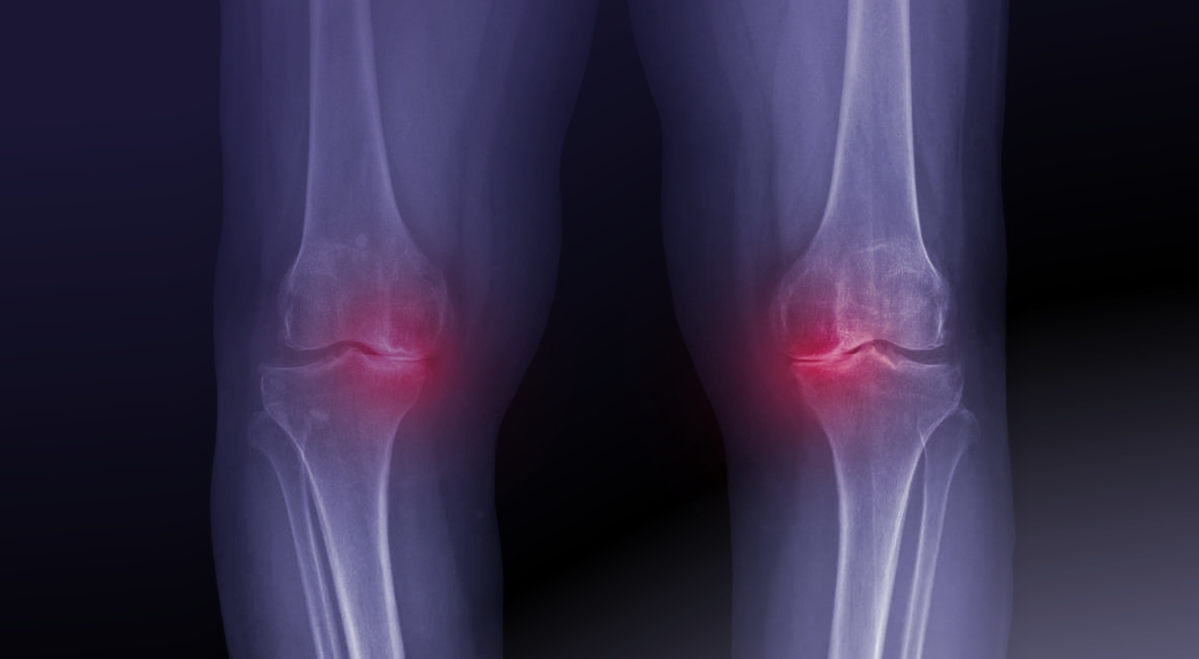
Total knee arthroplasty is increasingly common worldwide, but many patients still struggle with moderate to severe postoperative pain. Femoral nerve block is a widely used strategy to manage this pain, and interest has grown in whether adding dexmedetomidine—a sedative-analgesic agent—can further improve outcomes. Across six randomized trials, dexmedetomidine as an adjuvant offered small but consistent reductions in pain during movement and modest benefits at rest, along with lower opioid requirements. These improvements, however, did not exceed minimal clinically important thresholds. Safety outcomes were similar between groups, with no increase in hypotension, bradycardia, or nausea. Overall, adding dexmedetomidine appears to enhance analgesia without added risk, though the clinical impact remains modest and more high-quality research is needed.
Unlock the Full original article
You have access to 4 more FREE articles this month.
Click below to unlock and view this original article
Unlock Now
Critical appraisals of the latest, high-impact randomized controlled trials and systematic reviews in orthopaedics
Access to OrthoEvidence podcast content, including collaborations with the Journal of Bone and Joint Surgery, interviews with internationally recognized surgeons, and roundtable discussions on orthopaedic news and topics
Subscription to The Pulse, a twice-weekly evidence-based newsletter designed to help you make better clinical decisions
Exclusive access to original content articles, including in-house systematic reviews, and articles on health research methods and hot orthopaedic topics
Or upgrade today and gain access to all OrthoEvidencecontent for as little as $1.99 per week.
Already have an account? Log in
Are you affiliated with one of our partner associations?
Click here to gain complimentary access as part your association member benefits!