No radiographic or clinical benefit of patient specific instrumentation in TKA
No radiographic or clinical benefit of patient specific instrumentation in TKA
Patient-specific instrumentation does not improve radiographic alignment or clinical outcomes after total knee arthroplasty
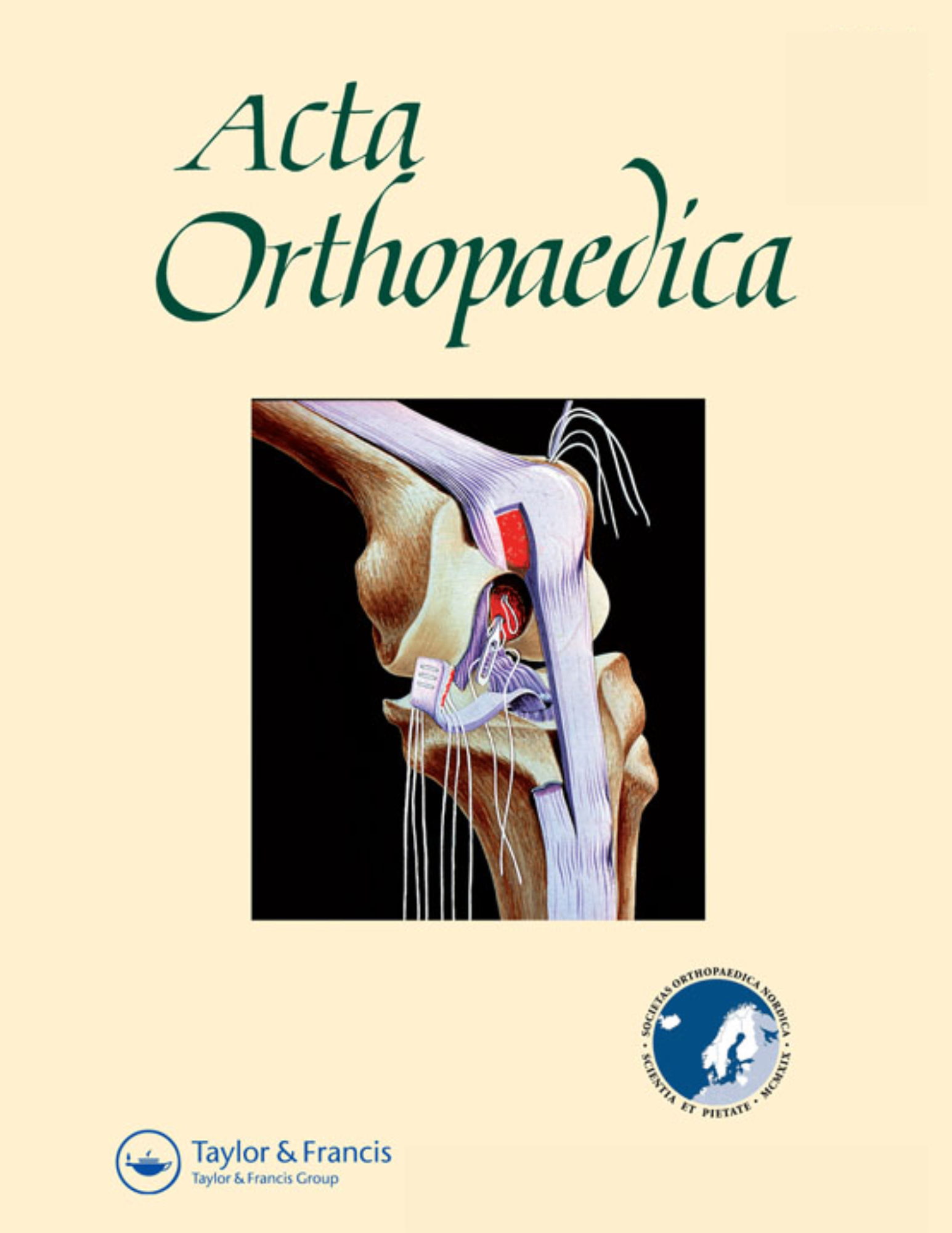
Acta Orthop. 2016 Aug;87(4):386-94Synopsis
21 studies evaluating the use of patient-specific instrumentation in total knee arthroplasty were included in this meta-analysis and systematic review. Pooled analyses demonstrated no significant difference between patient-specific instrumentation systems and conventional instruments in the incidence of excessive malalignment (>3 degrees deviation) in hip-knee-ankle angle. Additionally, the incidence of femoral component outliers in the coronal, sagittal, and axial planes, and tibial component outliers in the sagittal plane did not significantly differ, while tibial component outliers in the coronal plane occurred significantly more often with patient-specific instrumentation. No significant differences were found in short-term (3-month) clinical outcome measures. Two analyses which did favour patient-specific instrumentation were a lower number of surgical trays required during the procedure and shorter length of stay.
Were the search methods used to find evidence (original research) on the primary question or questions stated?
Was the search for evidence reasonably comprehensive?
Were the criteria used for deciding which studies to include in the overview reported?
Was the bias in the selection of studies avoided?
Were the criteria used for assessing the validity of the included studies reported?
Was the validity of all of the studies referred to in the text assessed with use of appropriate criteria (either in selecting the studies for inclusion or in analyzing the studies that were cited)?
Were the methods used to combine the findings of the relevant studies (to reach a conclusion) reported?
Were the findings of the relevant studies combined appropriately relative to the primary question that the overview addresses?
Were the conclusions made by the author or authors supported by the data and or analysis reported in the overview?
How would you rate the scientific quality of this evidence?
Yes = 1
Uncertain = 0.5
Not Relevant = 0
No = 0
The Reporting Criteria Assessment evaluates the transparency with which authors report the methodological and trial characteristics of the trial within the publication. The assessment is divided into five categories which are presented below.
4/4
Introduction
4/4
Accessing Data
4/4
Analysing Data
4/4
Results
3/4
Discussion
Detsky AS, Naylor CD, O'Rourke K, McGeer AJ, L'Abbé KA. J Clin Epidemiol. 1992;45:255-65
The Fragility Index is a tool that aids in the interpretation of significant findings, providing a measure of strength for a result. The Fragility Index represents the number of consecutive events that need to be added to a dichotomous outcome to make the finding no longer significant. A small number represents a weaker finding and a large number represents a stronger finding.
Why was this study needed now?
Patient-specific instrumentation (PSI) for component implantation in total knee arthroplasty is a recently-developed technology, with a number of randomized controlled trials performed investigating the systems of major orthopaedic device companies. PSI systems were designed to improve component alignment in these procedures, though conclusions on efficacy from previous studies vary widely. A synthesis of the literature was therefore needed to assess the current status of the role of PSI in TKA procedures.
What was the principal research question?
In total knee arthroplasty, are there any significant differences in radiographic alignment accuracy of component placement, perioperative parameters (blood loss, operative time, etc), and patient-reported outcome measures between patient-specific instrumentation and conventional instrumentation?
What were the important findings?
- There was no significant difference in the incidence of outliers in hip-knee-ankle angle (>3deg deviation from neutral) overall between patient-specific and conventional instruments (13 studies; RR 1.02 [95%CI 0.82-1.27]; p=0.86), or when specific products (PSI-Zimmer, Signature-Biomet, TruMatch-DePuy, Visionaire-Smith & Nephew) were analyzed as subgroups (all p>0.05).
- There was no significant difference between groups in the incidence of femoral component outliers in the coronal plane (11 studies; RR 0.81 [95%CI 0.6-1.09]). The incidence of tibial component outliers in the coronal plane was significantly higher among patient specific groups (11 studies; RR 1.64 [95%CI 1.12-2.42]).
- There were no significant differences between groups in the incidence of outliers in the sagittal plane of either the femoral component (8 studies; RR 0.97 [95%CI 0.82-1.15]) or the tibial component (8 studies; RR 1.47 [95%CI 0.97-2.23]).
- There was no significant difference between groups in the incidence of femoral component rotational outliers (6 studies; RR 0.80 [95%CI 0.52-1.23]).
- No significant difference between patient-specific and conventional instrumentation groups was observed in operative time (12 studies; MD -0.90min [95%CI -4.78, 2.98]; p=0.65) or tourniquet time (3 studies; MD -6min [95%CI -21.2, 10.1]). No significant differences were observed in analyses of intra-, postoperative, and total perioperative blood loss.
- The length of hospital stay was shortened by 8 hours (95%CI 3.1-12.5) following the use of patient-specific instrumentation versus conventional instrumentation.
- Two studies demonstrated a significantly lower use of surgical trays (MD 4 trays [95%CI 2.58-5.61]) with patient-specific versus conventional instrumentation.
- No significant differences between groups were observed in patient-reported outcome measures at 3 months, including Knee Society Scores and Oxford Knee Scores.
What should I remember most?
In total knee arthroplasty, the use of patient-specific instrumentation did not significantly reduce the incidence of malalignment overall, or of individual components in the coronal, sagittal, and axial planes. In fact, the incidence of tibial component outliers in the coronal plane was significantly higher following TKA with patient-specific instrumentation. No significant differences were observed in analyses of operative time, blood loss, or short-term clinical outcome. Advantages with the use of patient-specific instrumentation were noted concerning the number of surgical trays during the procedure, as well as in length of hospital stay.
How will this affect the care of my patients?
The results of this study suggest that there is no radiographic or clinical advantage to the use of patient-specific instrumentation in total knee arthroplasty, and in fact may compromise alignment of the tibial component. Benefits of patient-specific instrumentation appear limited to parameters of resource consumption, as evidenced by the analyses on surgical trays and the short, but significant, reduction in hospital stay. An economic analysis is needed to determine if these improvements in efficiency off-set the cost of the patient-specific instrumentation technology itself, as well as the preoperative imaging required to make the technology.
Learn about our AI Driven
High Impact Search Feature
Our AI driven High Impact metric calculates the impact an article will have by considering both the publishing journal and the content of the article itself. Built using the latest advances in natural language processing, OE High Impact predicts an article’s future number of citations better than impact factor alone.
Continue
 LOGIN
LOGIN

Join the Conversation
Please Login or Join to leave comments.