
 ARTHROPLASTY
ARTHROPLASTY
 GENERAL ORTHOPAEDICS
GENERAL ORTHOPAEDICS
 GENERAL ORTHOPAEDICS
GENERAL ORTHOPAEDICS
 PHYSIO & REHAB
PHYSIO & REHAB
 OSTEOARTHRITIS
OSTEOARTHRITIS
 RESEARCH
RESEARCH
 RESEARCH
RESEARCH
 SPORTS MEDICINE
SPORTS MEDICINE
 FOOT & ANKLE
FOOT & ANKLE
 RESEARCH
RESEARCH
 GENERAL ORTHOPAEDICS
GENERAL ORTHOPAEDICS
 SHOULDER & ELBOW
SHOULDER & ELBOW
 PHYSIO & REHAB
PHYSIO & REHAB
 ARTHROPLASTY
ARTHROPLASTY
 OSTEOARTHRITIS
OSTEOARTHRITIS
 RESEARCH
RESEARCH


AI in Clinical Research: Wins & Warning Signs
Artificial intelligence is rapidly reshaping clinical research, offering both transformative opportunities and important cautions. This article explores how generative AI is already improving core elements of clinical trials, including patient recruitment, eligibility screening, trial design, simulation, and the use of digital twins. Emerging evidence suggests AI can reduce screening time, enhance equity, and improve trial efficiency, while early applications in drug discovery hint at faster and more productive development pipelines. However, these advances are tempered by significant limitations. Ethical concerns surrounding data privacy, intellectual property, transparency, and bias remain unresolved, and successful computational predictions do not always translate into real-world clinical benefit. Overall, the article provides a balanced, evidence-informed view of where AI is delivering value today—and where careful oversight, validation, and governance are still essential as the technology continues to evolve.

Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR): New Promise for ACL Repair?
Anterior Cruciate Ligament (ACL) repair versus reconstruction–which is best for surgically indicated patients with ACL tears? For the last few decades at least, the answer has largely been reconstruction. It comes as no surprise, after all, ACL reconstruction has a much larger evidence base and proven track record. Ultimately, reconstructing the ACL results in a stable tissue less prone to retear. Yet, even gold standards have room to improve. ACL reconstructions, for example, often require autograft harvesting which can mean patients are left with donor site morbidity and pain – and longer recovery times. (1-3) The non-native tissue also lacks the biological properties of the native ACL which could inhibit the recovery of proprioceptive capabilities. (1-3) The procedure also requires larger, more invasive bone tunnels which can put patients at risk of developing early onset osteoarthritis. (1-3) All things that could be avoided, or minimized, through conservative management or ACL repair. This discussion is further complicated by other factors such as tear type, age, activity level, physical therapy protocol, and a relatively new array of alternative surgical procedures – which approach benefits select patients most? In this OE Original, we explore some of the evidence comparing ACL repair to reconstruction and discuss one new approach to ACL repair, Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR), that could reignite this debate once more.

Personalized Joint Replacement Surgery: The Hype, Hope & Hard Evidence
Instead of the typical “one-size-fits-all” approach to patient care, personalized medicine aims to improve clinical outcomes, reduce complications, and enhance patient satisfaction by tailoring treatment strategies to the unique genetic, anatomical, and lifestyle characteristics of each patient. As healthcare systems increasingly prioritize individualized care, surgical disciplines like orthopedics are beginning to embrace this paradigm shift.
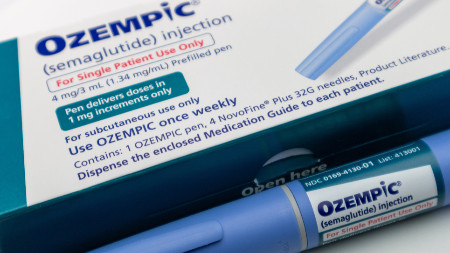
Ozempic in Orthopedics: Weight Loss Miracle or a Musculoskeletal Risk?
GLP-1 receptor agonists such as semaglutide and liraglutide have surged in popularity for weight loss, prompting growing interest in their musculoskeletal effects. Evidence suggests potential benefits for patients with osteoarthritis, including symptom improvement and reduced need for arthroplasty, though some data indicate a possible increased OA risk in those without prior disease. GLP-1 RAs may also reduce bone mineral density, yet paradoxically appear to lower fracture risk in individuals with type 2 diabetes. In surgical settings, GLP-1 use has been linked to fewer complications after hip and knee arthroplasty, but may raise perioperative risks in shoulder surgery. Overall, these medications show promise but require cautious use and further long-term study to clarify their impact on bone and joint health.

OE Top Trends for 2025
Orthopaedic research in 2024 marked a shift in focus, with extremity care and sports medicine drawing more attention than arthroplasty. Landmark studies highlighted iodine-alcohol antisepsis reducing surgical site infections, combined strength and balance training improving chronic ankle instability, and rapid rehabilitation lowering complications after hip fractures. Explorers—those at the forefront of research—showed heightened interest in platelet-rich plasma formulations, digital rehabilitation strategies, and long-term outcomes of surgical innovations. Looking to 2025, the field is set to expand into AI-assisted imaging and diagnostics, 3D-printed custom implants, and the growing role of digitized care. Meanwhile, GLP-1 therapies for weight loss may emerge as powerful tools in perioperative management and osteoarthritis prevention. Together, these trends suggest a rapidly evolving landscape where biologics, technology, and digital health converge to redefine musculoskeletal care.
Meet our Association Partners
OrthoEvidence is committed to establishing a culture of evidence-based decision making within the healthcare industry.
Learn More






















OE Subscriptions
Curated content directly to your inbox.Exclusive Interviews
Go behind the scenes and gain insight from the authors.Conference Reports
Missed the conference? Catch up with our presentation and abstract summaries.Ask OE
Have questions on a condition, treatment, or outcome? OE’s AI delivers the evidence-based answers, you’re looking for.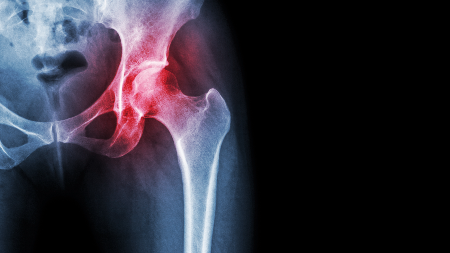
Certain Subsets of Older Patients With Pelvic Ring Injuries Benefit From Surgery

Smith+Nephew to Acquire Integrity Ortho for Up to $450M

Integrating Medical Records With AI 'a watershed moment' in medicine - is it dangerous?

Round table: Experts discuss role of AI in orthopedics
Start your free trial today
Expand your perspective with high-quality evidence!





















































