FOOT & ANKLE
FOOT & ANKLE
 RESEARCH
RESEARCH
 PERSONAL GROWTH
PERSONAL GROWTH
 SHOULDER & ELBOW
SHOULDER & ELBOW
 PEDIATRIC ORTHOPAEDICS
PEDIATRIC ORTHOPAEDICS
 OSTEOARTHRITIS
OSTEOARTHRITIS
 ARTHROPLASTY
ARTHROPLASTY
 INNOVATION
INNOVATION
 INNOVATION
INNOVATION
 SHOULDER & ELBOW
SHOULDER & ELBOW
 SPINE
SPINE
 RESEARCH
RESEARCH
 RESEARCH
RESEARCH
 SHOULDER & ELBOW
SHOULDER & ELBOW
 GENERAL ORTHOPAEDICS
GENERAL ORTHOPAEDICS
 RESEARCH
RESEARCH


Blades, Body Checks, and Broken Bones: The Unavoidable Cost of Playing in the NHL
Injury is an unavoidable reality in elite sport, and the NHL is no exception. Strains and sprains are common across athletics, while fractures and concussions remain significant risks in professional hockey. Lower-body injuries account for a substantial share of reported cases, with hip and pelvic injuries—particularly labral tears—frequently linked to body checking. Shoulder injuries such as Bankart lesions also contribute to missed games. Although protective equipment like helmets and visors eventually became mandatory, resistance continues around neck guards despite documented fatal incidents. Ultimately, injuries can be reduced through equipment, conditioning, and rule enforcement, but never fully eliminated.

The Silent Epidemic: Rising Senior Fall Rates and What Clinicians Must Act On Now
Falls remain the leading cause of injury-related death among adults aged sixty-five and older, with risk rising sharply with advancing age. Mortality rates vary substantially by sex, race, and geography, reflecting broader socioeconomic and healthcare disparities. White older adults consistently show higher fatal fall rates, while rates differ across other racial groups and states. Ankle and foot injuries are common and can both result from and contribute to falls. Contributing factors include medication effects, balance deficits, muscle weakness, vision changes, chronic disease, and environmental hazards. Prevention strategies emphasize medication review, strength and balance training, physiotherapy, and appropriate footwear to reduce injury risk and long-term burden.

AI in Clinical Research: Wins & Warning Signs
Artificial intelligence is rapidly reshaping clinical research, offering both transformative opportunities and important cautions. This article explores how generative AI is already improving core elements of clinical trials, including patient recruitment, eligibility screening, trial design, simulation, and the use of digital twins. Emerging evidence suggests AI can reduce screening time, enhance equity, and improve trial efficiency, while early applications in drug discovery hint at faster and more productive development pipelines. However, these advances are tempered by significant limitations. Ethical concerns surrounding data privacy, intellectual property, transparency, and bias remain unresolved, and successful computational predictions do not always translate into real-world clinical benefit. Overall, the article provides a balanced, evidence-informed view of where AI is delivering value today—and where careful oversight, validation, and governance are still essential as the technology continues to evolve.

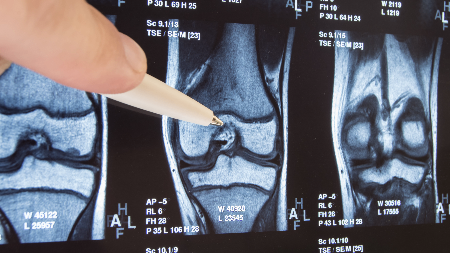
Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR): New Promise for ACL Repair?
Anterior Cruciate Ligament (ACL) repair versus reconstruction–which is best for surgically indicated patients with ACL tears? For the last few decades at least, the answer has largely been reconstruction. It comes as no surprise, after all, ACL reconstruction has a much larger evidence base and proven track record. Ultimately, reconstructing the ACL results in a stable tissue less prone to retear. Yet, even gold standards have room to improve. ACL reconstructions, for example, often require autograft harvesting which can mean patients are left with donor site morbidity and pain – and longer recovery times. (1-3) The non-native tissue also lacks the biological properties of the native ACL which could inhibit the recovery of proprioceptive capabilities. (1-3) The procedure also requires larger, more invasive bone tunnels which can put patients at risk of developing early onset osteoarthritis. (1-3) All things that could be avoided, or minimized, through conservative management or ACL repair. This discussion is further complicated by other factors such as tear type, age, activity level, physical therapy protocol, and a relatively new array of alternative surgical procedures – which approach benefits select patients most? In this OE Original, we explore some of the evidence comparing ACL repair to reconstruction and discuss one new approach to ACL repair, Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR), that could reignite this debate once more.

Personalized Joint Replacement Surgery: The Hype, Hope & Hard Evidence
Instead of the typical “one-size-fits-all” approach to patient care, personalized medicine aims to improve clinical outcomes, reduce complications, and enhance patient satisfaction by tailoring treatment strategies to the unique genetic, anatomical, and lifestyle characteristics of each patient. As healthcare systems increasingly prioritize individualized care, surgical disciplines like orthopedics are beginning to embrace this paradigm shift.
Meet our Association Partners
OrthoEvidence is committed to establishing a culture of evidence-based decision making within the healthcare industry.
Learn More



























OE Subscriptions
Curated content directly to your inbox.Exclusive Interviews
Go behind the scenes and gain insight from the authors.Conference Reports
Missed the conference? Catch up with our presentation and abstract summaries.Ask OE
Have questions on a condition, treatment, or outcome? OE’s AI delivers the evidence-based answers, you’re looking for.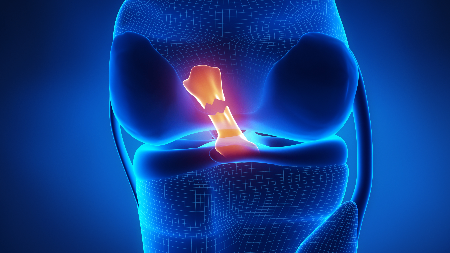
New Implants Seek to Close the Treatment Gap for Meniscus Tears
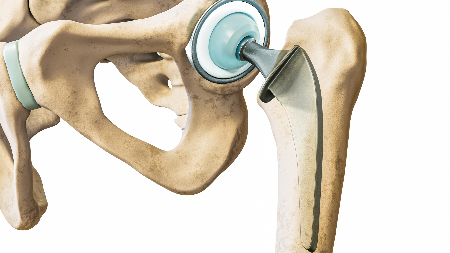
Zimmer Biomet Earns 510(k) for G7 TM Acetabular System

The Keys to Unlocking Improved 3D-printed Lattice Designs
Disruptive Technology for the Joint Replacement Market
Start your free trial today
Expand your perspective with high-quality evidence!