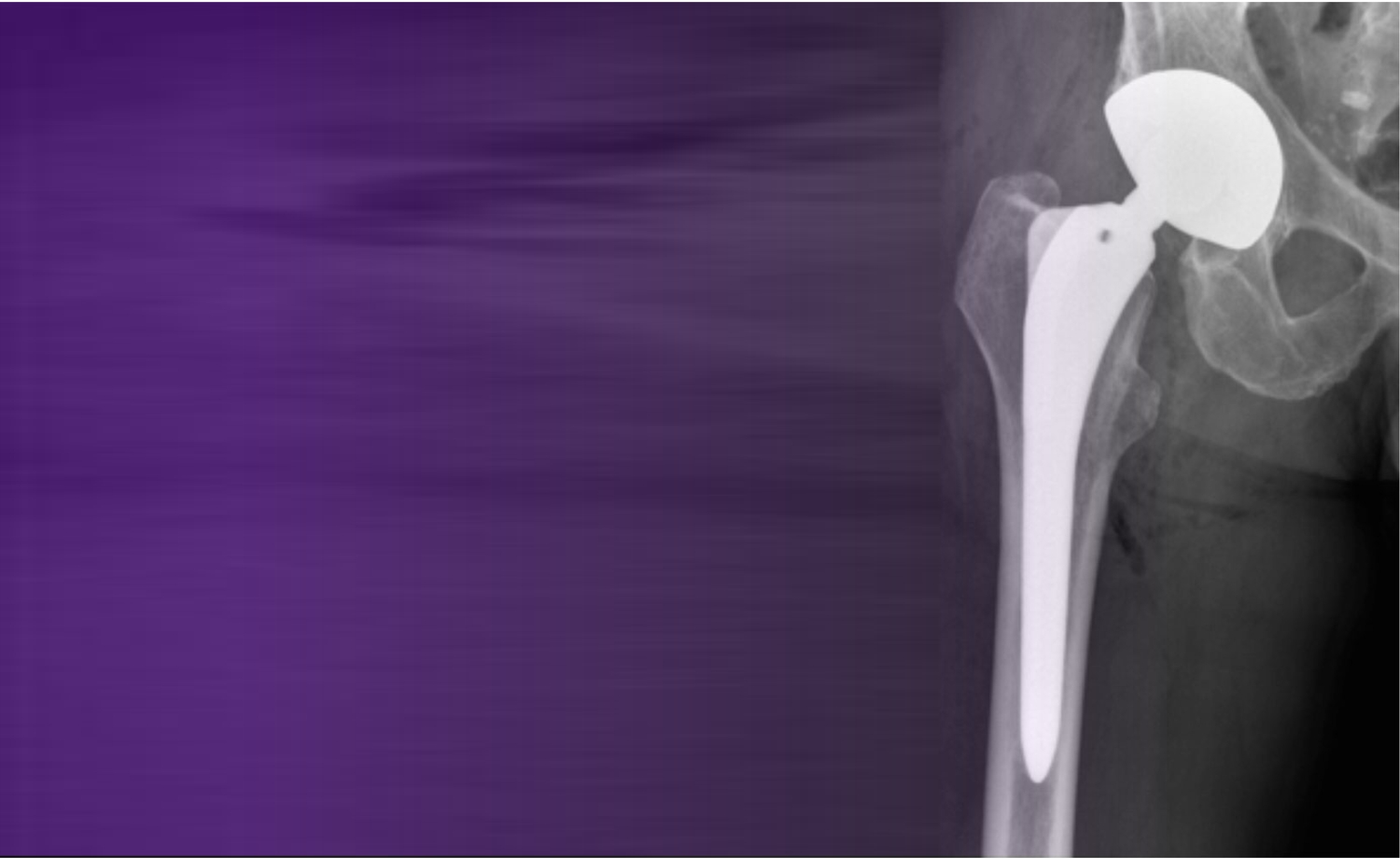
The Use of Dual Mobility Implants in Primary Total Hip Arthroplasty .
Dual mobility implants, first introduced in 1974, aim to reduce dislocation in total hip arthroplasty (THA) by combining low-friction and high-range-of-motion designs. Though widely used in revision THA, recent literature explores their role in primary THA, particularly in high-risk groups such as those with femoral neck fractures or reduced spinopelvic mobility. Evidence suggests reduced dislocation risk and improved function, but most studies are observational or limited by short follow-up. Concerns remain over implant-specific risks like intraprosthetic dislocation and metal ion levels. While early results are promising in select patients, routine use in all primary THAs remains unsupported without stronger, long-term evidence.
Unlock the Full original article
You have access to 4 more FREE articles this month.
Click below to unlock and view this original article
Unlock Now
Critical appraisals of the latest, high-impact randomized controlled trials and systematic reviews in orthopaedics
Access to OrthoEvidence podcast content, including collaborations with the Journal of Bone and Joint Surgery, interviews with internationally recognized surgeons, and roundtable discussions on orthopaedic news and topics
Subscription to The Pulse, a twice-weekly evidence-based newsletter designed to help you make better clinical decisions
Exclusive access to original content articles, including in-house systematic reviews, and articles on health research methods and hot orthopaedic topics
Or upgrade today and gain access to all OrthoEvidencecontent for as little as $1.99 per week.
Already have an account? Log in
Are you affiliated with one of our partner associations?
Click here to gain complimentary access as part your association member benefits!