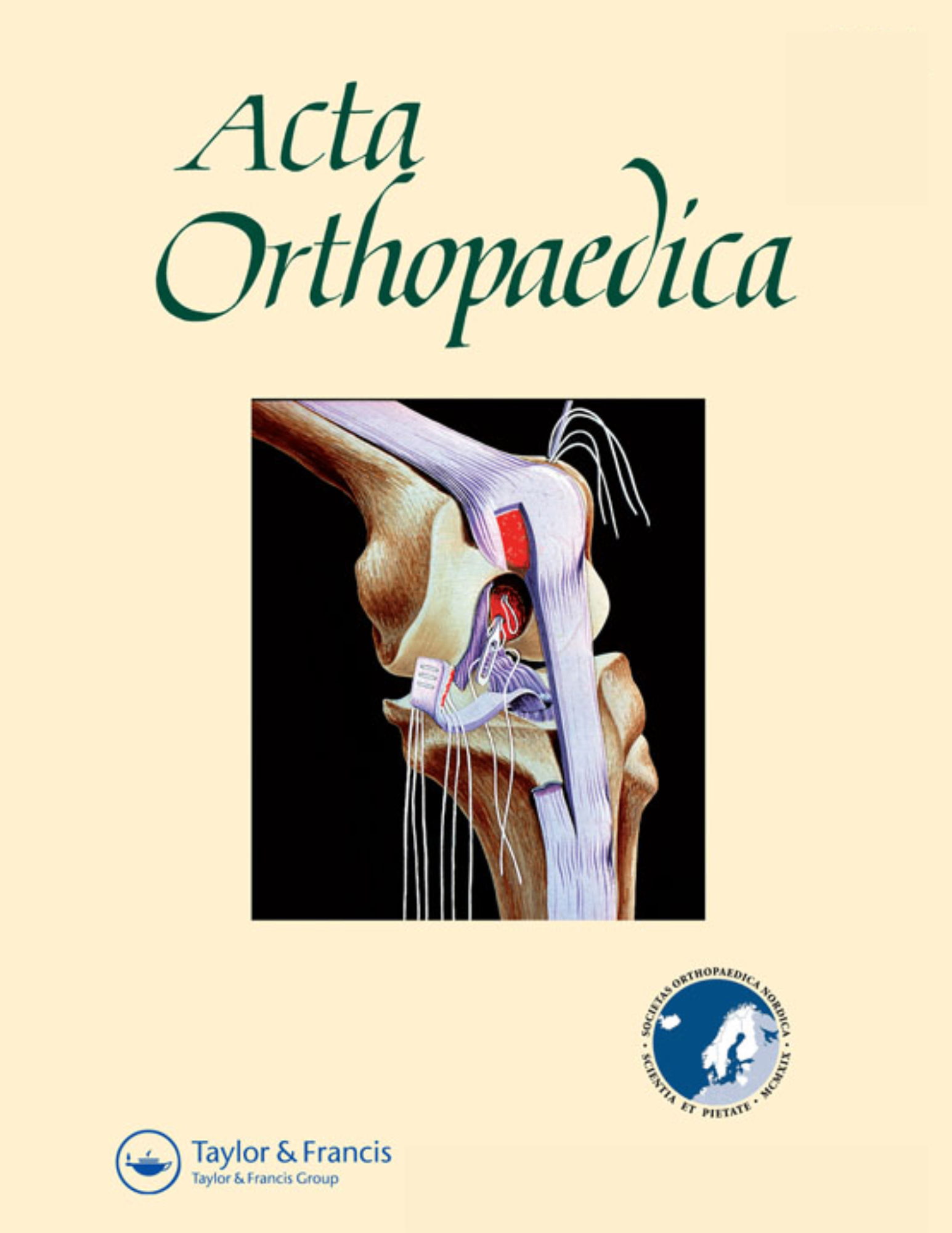
Muller vs. Virtec straight stem shape comparable for long-term radiological change in THR .
Similar effect of stem geometry on radiological changes with 2 types of cemented straight stem
Acta Orthop. 2016 Apr;87(2):120-5.646 patients (711 hips) patients undergoing primary total hip replacement with straight femoral stem cement fixation were randomized to receive either a Muller straight stem (MSS) or the Virtec straight stem (VSS) for the purpose of comparing long-term radiographical and survival success ten years post-surgery. Results demonstrated that patients in both groups had comparable implant survival, osteolysis, subsidence, and debonding rates at 10 years.
Unlock the Full ACE Report
You have access to 4 more FREE articles this month.
Click below to unlock and view this ACE Reports
Unlock Now
Critical appraisals of the latest, high-impact randomized controlled trials and systematic reviews in orthopaedics
Access to OrthoEvidence podcast content, including collaborations with the Journal of Bone and Joint Surgery, interviews with internationally recognized surgeons, and roundtable discussions on orthopaedic news and topics
Subscription to The Pulse, a twice-weekly evidence-based newsletter designed to help you make better clinical decisions
Exclusive access to original content articles, including in-house systematic reviews, and articles on health research methods and hot orthopaedic topics
Or upgrade today and gain access to all OrthoEvidencecontent for as little as $1.99 per week.
Already have an account? Log in
Are you affiliated with one of our partner associations?
Click here to gain complimentary access as part your association member benefits!