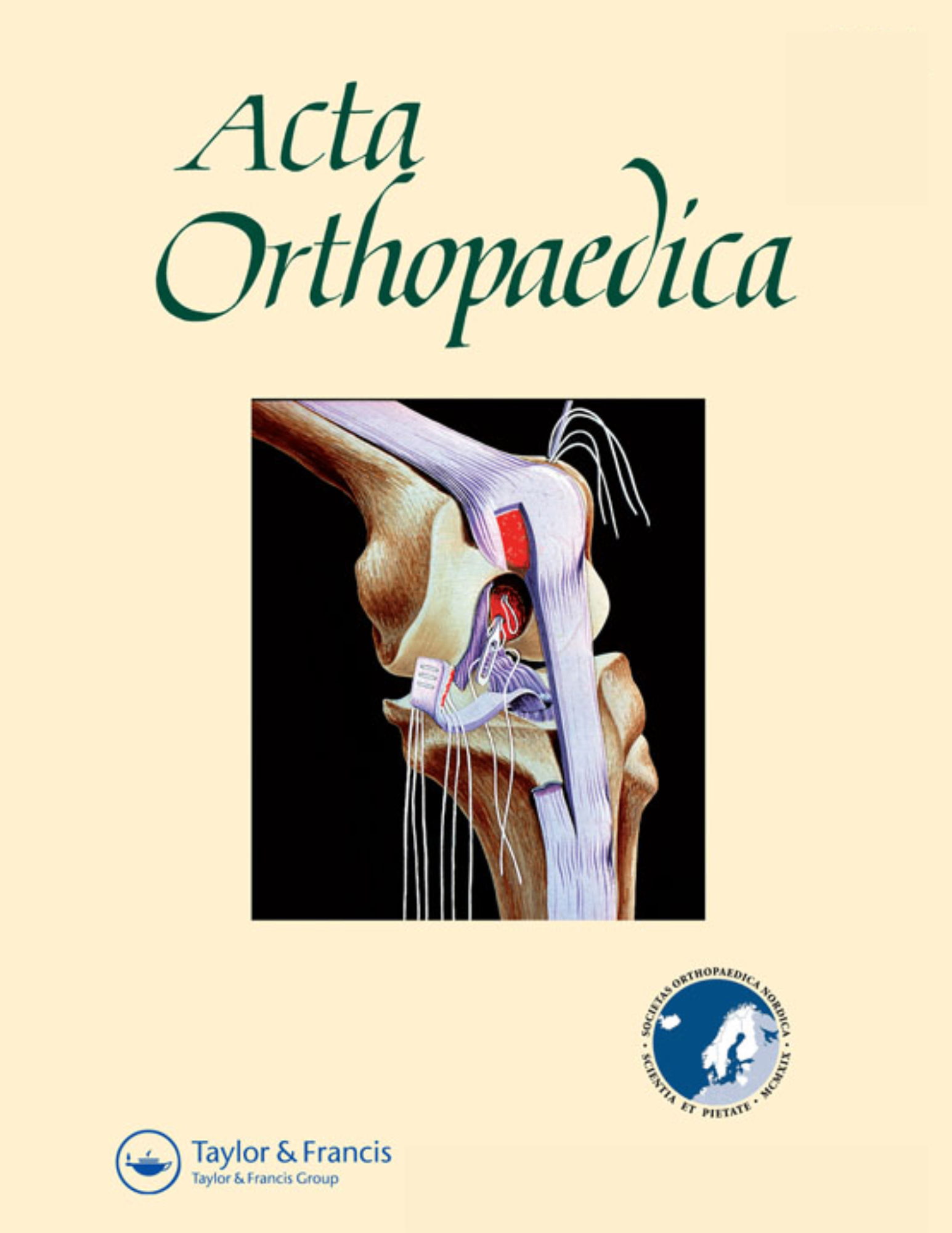
The effect of different hydroxyapatite application techniques on femoral stem stability
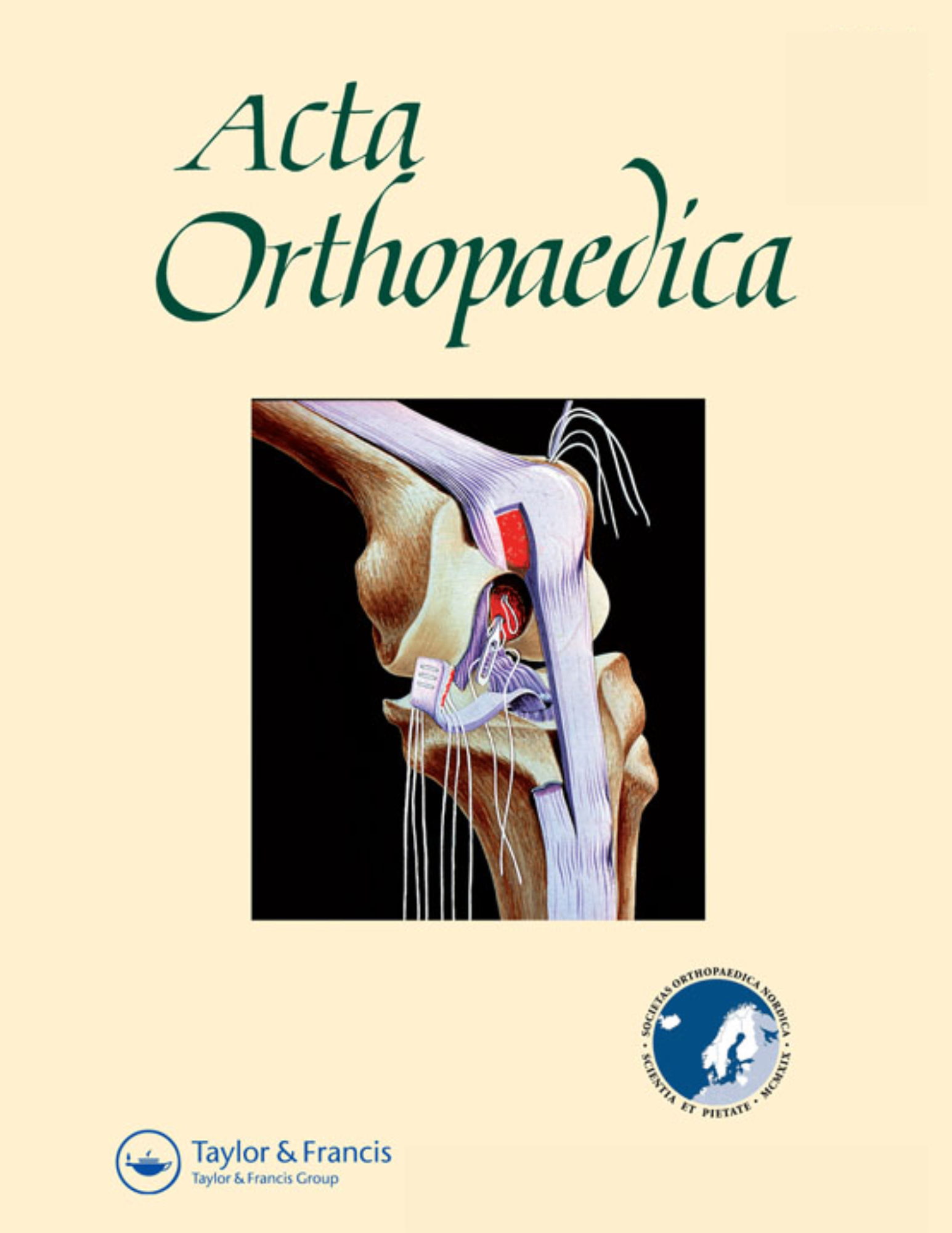
The effect of different hydroxyapatite application techniques on femoral stem stability
No medium-term advantage of electrochemical deposition of hydroxyapatite in cementless femoral stems
Acta Orthop. 2016 Feb;87(1):42-7.Did you know you're eligible to earn 0.5 CME credits for reading this report? Click Here
Synopsis
50 patients (55 hips) scheduled for primary total hip arthroplasty were randomized to receive implants with hydroxyapatite applied either via electrochemical deposition or plasma-spray. The purpose of this study was to determine whether differences exists between methods with respect to bone density loss, aseptic loosening, periprosthetic migration and functional scores when evaluated up to 5 years post-surgery. Results demonstrated that although patients in the plasma-spray group demonstrated significantly less loss in bone mineral density and decreased retroversion rates at certain time-points, the two methods of hydroxyapatite application were deemed to be clinically comparable.
Was the allocation sequence adequately generated?
Was allocation adequately concealed?
Blinding Treatment Providers: Was knowledge of the allocated interventions adequately prevented?
Blinding Outcome Assessors: Was knowledge of the allocated interventions adequately prevented?
Blinding Patients: Was knowledge of the allocated interventions adequately prevented?
Was loss to follow-up (missing outcome data) infrequent?
Are reports of the study free of suggestion of selective outcome reporting?
Were outcomes objective, patient-important and assessed in a manner to limit bias (ie. duplicate assessors, Independent assessors)?
Was the sample size sufficiently large to assure a balance of prognosis and sufficiently large number of outcome events?
Was investigator expertise/experience with both treatment and control techniques likely the same (ie.were criteria for surgeon participation/expertise provided)?
Yes = 1
Uncertain = 0.5
Not Relevant = 0
No = 0
The Reporting Criteria Assessment evaluates the transparency with which authors report the methodological and trial characteristics of the trial within the publication. The assessment is divided into five categories which are presented below.
2/4
Randomization
3/4
Outcome Measurements
4/4
Inclusion / Exclusion
4/4
Therapy Description
4/4
Statistics
Detsky AS, Naylor CD, O'Rourke K, McGeer AJ, L'Abbé KA. J Clin Epidemiol. 1992;45:255-65
The Fragility Index is a tool that aids in the interpretation of significant findings, providing a measure of strength for a result. The Fragility Index represents the number of consecutive events that need to be added to a dichotomous outcome to make the finding no longer significant. A small number represents a weaker finding and a large number represents a stronger finding.
Why was this study needed now?
Fixation of implants following total hip arthroplasty is critically dependent on successful integration between prosthetic and natural surfaces. As such, osseointegrative techniques have been developed in order to ensure implant stability; this includes the application of naturally occurring and bone formation inducing biomaterial such as hydroxyapatite. Hydroxyapatite is normally applied via plasma spray or by electrochemical deposition for the purpose of reducing aseptic loosening and bone resorption, however, there is a lack of clinical evaluation that directly compares the two methods. Thus, the current study was conducted.
What was the principal research question?
For patients scheduled for total hip arthroplasty, did either hydroxyapatite application accomplished by electrochemical disposition or plasma-spray result in significantly reduced periprosthetic migration and bone resorption, when assessed up to 5 years postoperatively?
What were the important findings?
- Bone mineral density (BMD) was reported to have declined in all Gruen zones for all patients, with the majority of this bone loss occurring within the first year. After two years, bone loss ranged from 8-14% in zones 2 to 6 and ~30% in zone 7.
- The greatest loss in bone remodeling rate was seen in zone 7 (34% for BM group vs. 31% for HA group) and in zone 1 (20% for BM group vs. 25% for HA group).
- BMD for patients in the BM group decreased by a rate of 0.11%/month (95% CI -0.19 to -0.04), compared to a rate of 0.01%/month (95% CI -0.08 to 0.1) in the HA group; this difference was statistically significant (p=0.04), however, it was determined to be clinically irrelevant.
- Stem subsidence/migration during the first 3 months occurred at comparable rates when study groups were compared (p=0.6); subsidence rates were minuscule when measured after the 3-month time point, with comparable rates once again demonstrated between study groups (p=0.4).
- Rates of retroversion were significantly higher in the first three months for patients in the BM group when compared to the HA group (0.17 degrees/month [0.11-0.23] vs. 0.06 degrees/month [-0.01-0.12] respectively, p=0.006); after the 3-month time point, retroversion rates remained stable and were comparable between study groups (p=0.3).
- HHS and OHS scores were comparable between study groups after 5 postoperative years.
What should I remember most?
Bone mineral density loss and retroversion rates in THA patients significantly differed between electrochemical deposition and plasma-spray groups (significance was observed at 3 months for the latter), with less severe rates observed in patients who receive hydroxyapatite application through plasma-spray. However, as all patients and prostheses remained stable throughout the study period the significance was deemed to be clinically insignificant. All other outcomes were comparable when measured at all follow-up points.
How will this affect the care of my patients?
The results of this study demonstrated that there were no clinically significant differences between the two methods of hydroxyapatite application five years following total hip arthroplasty. While this study demonstrates no differences between hydroxyapatite application techniques, questions still remain regarding the use of hydroxyapatite and if it provides any clinically relevant advantages.
Learn about our AI Driven
High Impact Search Feature
Our AI driven High Impact metric calculates the impact an article will have by considering both the publishing journal and the content of the article itself. Built using the latest advances in natural language processing, OE High Impact predicts an article’s future number of citations better than impact factor alone.
Continue
 LOGIN
LOGIN

Join the Conversation
Please Login or Join to leave comments.